Atypical Chest Pain: What It Is and How to Handle It
Chest pain doesn’t always mean a heart attack. When the discomfort feels odd, vague, or shows up in strange places, doctors call it atypical chest pain. It can be scary, but not every case is life‑threatening. Knowing the usual culprits and red‑flag signs helps you decide whether a quick ER visit is needed or a follow‑up with your primary doctor will do.
Common Reasons Behind Atypical Chest Pain
Most of the time the pain comes from non‑cardiac sources. Here are the everyday triggers you’re likely to run into:
- Muscle strain: A sudden lift, a bad posture, or an intense workout can pull the intercostal muscles between the ribs, creating a sharp or aching feeling.
- Acid reflux (GERD): Stomach acid splashing up into the esophagus can mimic heart pain, especially after a big meal or lying down.
- Costochondritis: Inflammation where the ribs meet the breastbone often produces localized tenderness that worsens when you press on the area.
- Breathing issues: Asthma, pneumonia, or a pulled lung (pneumothorax) can cause sharp, stabbing pain that gets worse with deep breaths.
- Stress and anxiety: Panic attacks can trigger tightness in the chest, rapid heartbeat, and a feeling of pressure that mimics a heart problem.
Even though these causes are usually benign, they can still be painful and disrupt daily life. Treating the underlying issue—like using antacids for reflux or gentle stretches for muscle strain—often eases the discomfort.
When to Treat It as an Emergency
Some chest pains need immediate attention. If you notice any of the following, call 911 or head to the nearest ER right away:
- Sudden, crushing pressure that spreads to the arm, jaw, or back.
- Shortness of breath, sweating, or nausea that comes on fast.
- Pain that doesn’t improve after a few minutes of rest.
- History of heart disease, high blood pressure, or diabetes.
These signs point more toward a cardiac event than a harmless cause. Even if you’re unsure, it’s safer to get checked out.
For non‑emergent cases, start with these simple steps:
- Rest and calm down: Sit upright, take slow breaths, and avoid heavy activity.
- Track the pain: Note when it started, what you were doing, its intensity (1‑10), and anything that makes it better or worse.
- Try over‑the‑counter help: Antacids for reflux, ibuprofen for inflammation, or a warm compress for muscle soreness.
- Schedule a visit: If the pain persists for more than a few days, worsens, or returns frequently, see your doctor for an exam, EKG, or imaging.
During the appointment, be ready to share your pain diary. Doctors often start with a physical exam, check blood pressure, and may order an EKG or chest X‑ray to rule out heart or lung issues.
Bottom line: atypical chest pain is common and usually not a heart attack, but you can’t ignore it. Knowing the typical non‑cardiac reasons helps you act confidently, while staying alert for the warning signs that demand urgent care.
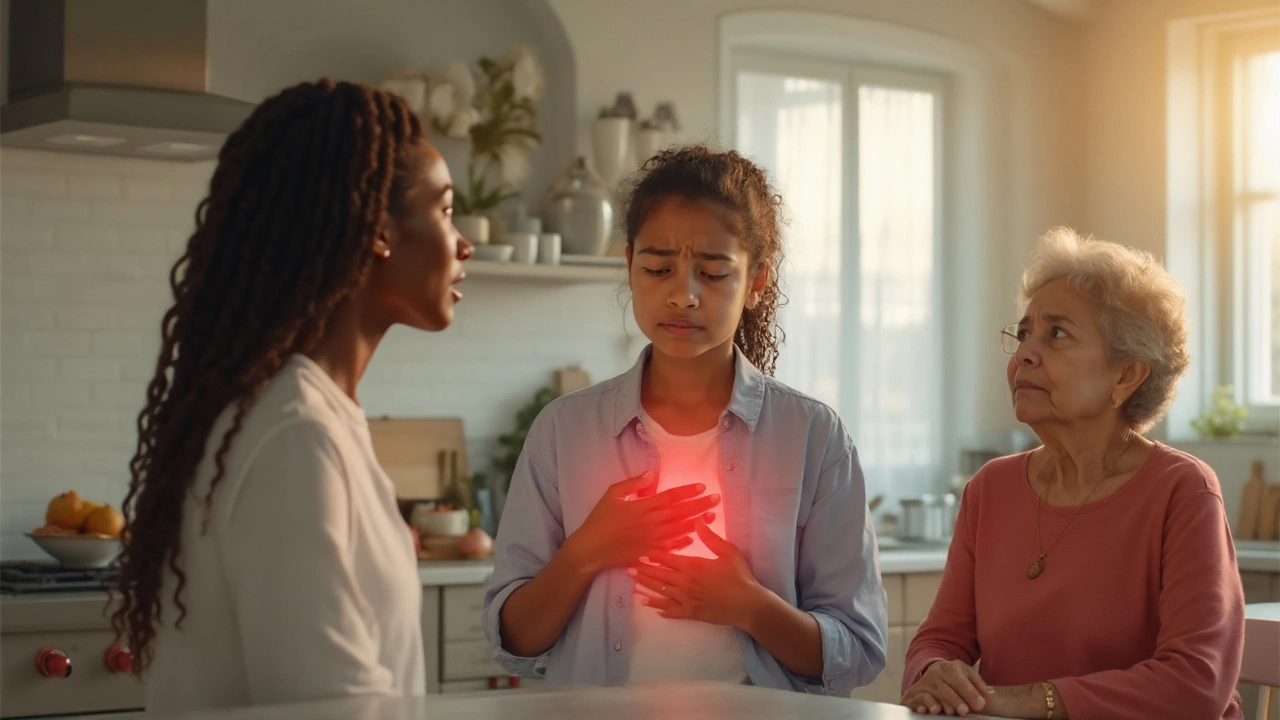
Women’s Chest Pain: Recognizing Unique Symptoms & Causes
Learn how chest pain shows up differently in women, its hidden causes, and what symptoms demand urgent care. Get practical tips for recognizing and responding to female‑specific heart warning signs.
Read More