Acid Indigestion – What It Is and How to Manage It
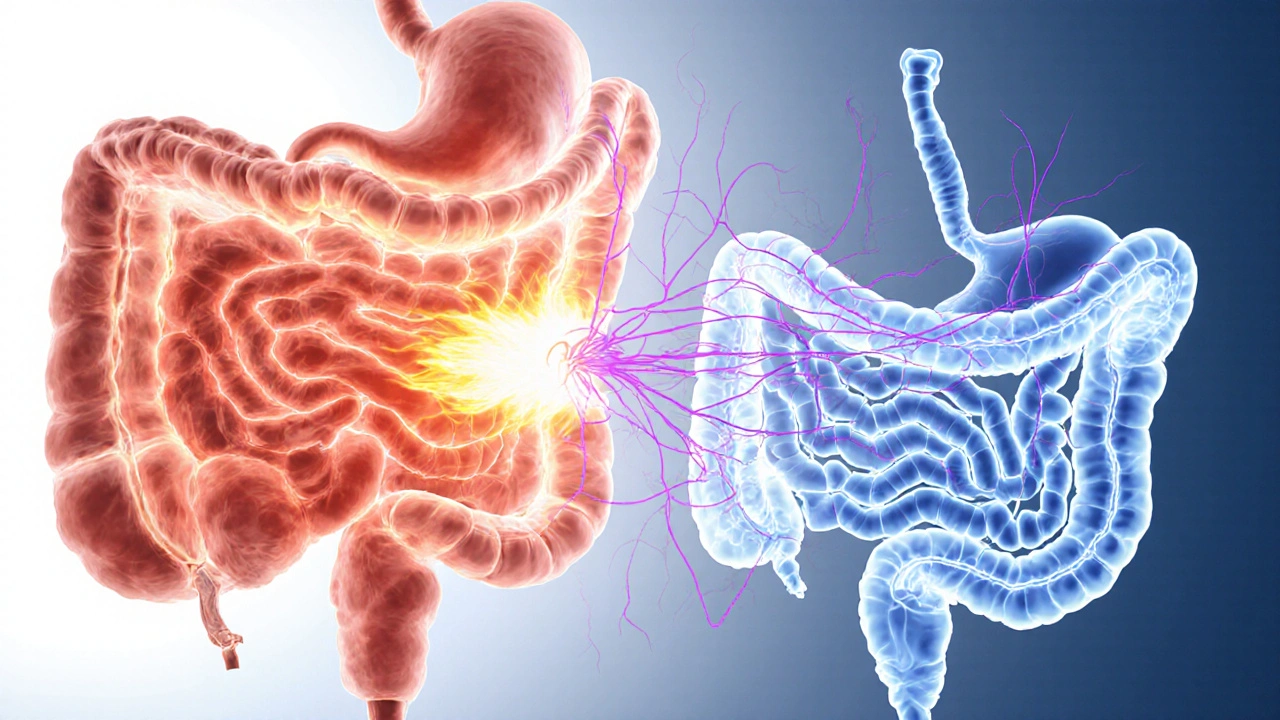
When working with acid indigestion, a burning sensation in the chest or throat caused by stomach acid flowing back into the esophagus. Also known as dyspepsia, it can range from an occasional annoyance to a chronic problem that disrupts daily life. Acid indigestion often shows up after big meals, spicy foods, or stress, and it signals that the digestive system needs a break. Understanding the basics helps you spot the pattern before the discomfort turns into a bigger issue.
One of the most common companions of acid indigestion is heartburn, a sharp, hot feeling that climbs the throat and may be triggered by the same acid reflux. Heartburn is essentially a symptom of the same process, so when you feel it, acid indigestion is likely present. Another related condition is GERD, gastroesophageal reflux disease, a chronic form of reflux that can damage the esophageal lining if untreated. GERD goes beyond occasional discomfort; it often requires medical monitoring and long‑term lifestyle changes. To calm the acid, many turn to antacids, medications that neutralize stomach acid quickly. They provide fast relief but don’t address underlying habits. Speaking of habits, dietary triggers, foods like caffeine, chocolate, citrus, and fatty meals that relax the lower esophageal sphincter play a big role in how often acid indigestion shows up. The triple relationship is clear: dietary triggers influence acid indigestion, acid indigestion includes heartburn, and persistent acid indigestion may develop into GERD, which often requires antacid therapy or prescription meds.
Practical Steps to Keep Acid Indigestion in Check
Start by watching what you eat and when you eat it. Smaller, more frequent meals keep the stomach from over‑producing acid, and avoiding the known triggers reduces the chance of the lower esophageal sphincter relaxing at the wrong time. Stay upright for at least an hour after meals—gravity helps keep acid where it belongs. Losing a few pounds if you’re carrying extra weight can lower abdominal pressure, which in turn lessens reflux episodes. If you smoke, cutting back or quitting makes a noticeable difference because nicotine also relaxes the sphincter. When you do need quick relief, antacids work in minutes, but consider using an H2 blocker or a proton‑pump inhibitor for longer‑term control if over‑the‑counter options aren’t enough. Finally, listen to your body; if the burning becomes frequent, severe, or accompanied by weight loss or vomiting, it’s time to talk to a healthcare professional. The articles below dive deeper into each of these topics, offering detailed comparisons of meds, lifestyle tweaks, and when to seek medical advice, so you can build a plan that works for you.
How Acid Indigestion Relates to IBS: Causes, Symptoms & Relief
Explore how acid indigestion and IBS are linked, uncover shared triggers, and learn combined strategies-diet, stress relief, and meds-to ease both conditions.
Read More