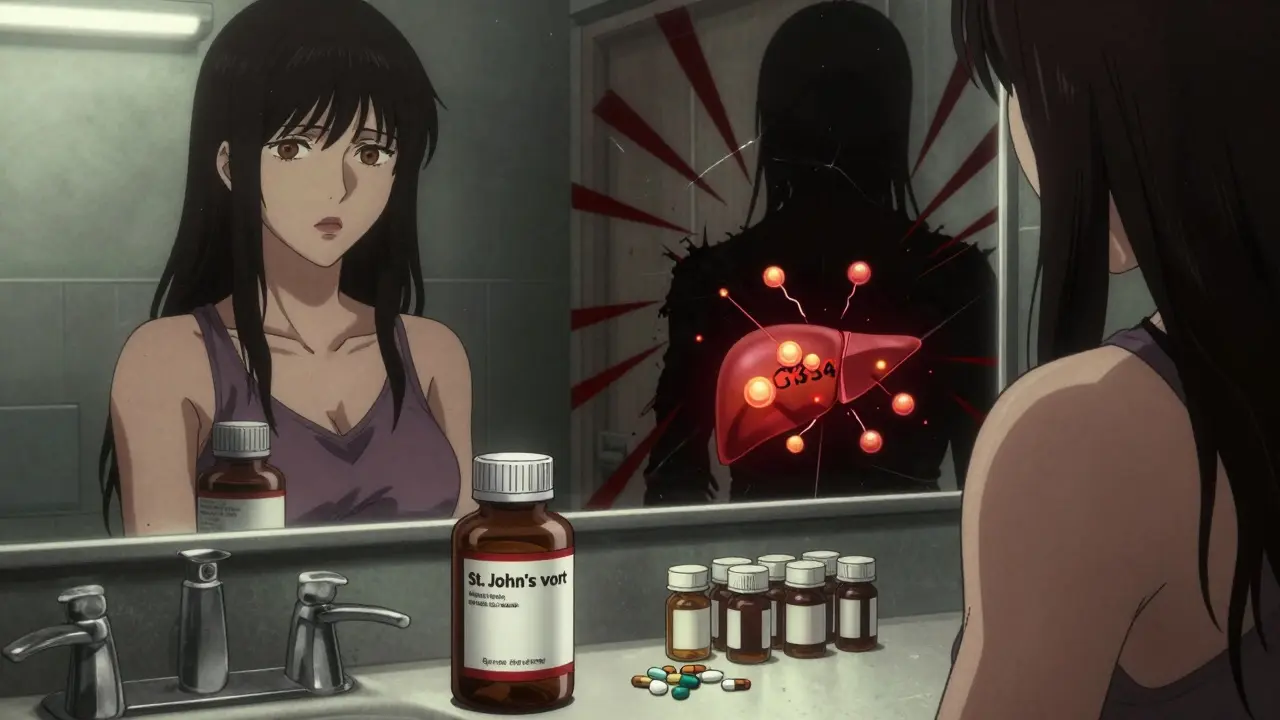
St. John’s Wort looks harmless. It’s sold in bottles next to vitamin D and omega-3s. The label says “natural,” and you might assume it’s safe-especially if you’re trying to avoid prescription antidepressants. But here’s the truth: St. John’s Wort can turn your life-saving medications into useless pills-or worse, make them dangerously strong. This isn’t theory. It’s happening in real people, every day.
How St. John’s Wort Changes How Your Body Handles Medication
St. John’s Wort doesn’t just float through your system. It actively rewires how your liver and intestines process drugs. The key player is hyperforin, a compound in the herb that turns on a set of enzymes called CYP3A4. These enzymes are like the body’s cleanup crew-they break down medications so they can be flushed out. When hyperforin wakes them up, they start working overtime. That means drugs get broken down too fast. Your blood levels drop. And if those drugs are keeping you alive, that’s a problem.
It’s not just enzymes. St. John’s Wort also kicks in P-glycoprotein, a transporter that pushes drugs out of cells. This affects everything from heart meds to HIV pills. Studies show that after just two weeks of taking 900 mg daily, CYP3A4 activity can spike by 40%. That’s enough to slash the effectiveness of many drugs by 30% to 50%.
Warfarin: A Deadly Combination
If you’re on warfarin (Coumadin) to prevent clots, mixing it with St. John’s Wort could land you in the ER. Warfarin needs to stay in your blood at a very tight range. Too low, and you risk a stroke or pulmonary embolism. Too high, and you bleed internally.
Case reports from Australia and Sweden show patients on stable warfarin doses suddenly dropping their INR-from a safe 2.5 down to 1.3-in less than a week after starting St. John’s Wort. That’s not a fluke. It’s a pattern. One patient’s INR dropped from 2.8 to 1.5 in 10 days. Doctors had to increase his warfarin dose by 25% just to get back to safety. The Therapeutic Goods Administration (TGA) logged 22 such cases between 1998 and 2000. These aren’t old stories. They’re warnings that still apply today.
Birth Control Failure: More Common Than You Think
Women taking oral contraceptives might think they’re protected. But St. John’s Wort can cut ethinyl estradiol levels by 25% to 35%. That’s enough to make birth control fail-even if you’ve never missed a pill.
One user on Drugs.com wrote: “I took St. John’s Wort for three weeks while on birth control. I had breakthrough bleeding. Then I found out I was pregnant.” There are 13 documented cases of unintended pregnancy linked to this interaction. It’s not rare. It’s predictable. And it’s avoidable.
Organ Transplant Patients at Risk
If you’ve had a kidney, liver, or heart transplant, you’re on immunosuppressants like cyclosporine or tacrolimus. These drugs keep your immune system from attacking your new organ. But they need to stay at precise levels. Too low? Rejection. Too high? Toxicity.
One transplant patient on HealthUnlocked shared: “My cyclosporine levels dropped 40% after I started St. John’s Wort. My doctor said I was hours away from organ rejection.” That’s not an exaggeration. Studies confirm cyclosporine levels can fall by 30% to 50% with St. John’s Wort use. One Australian case led to acute rejection. This isn’t a “maybe.” It’s a hard stop.

Antidepressants: The Serotonin Danger Zone
People take St. John’s Wort because they want to feel better. But if you’re already on an SSRI-like sertraline, fluoxetine, or citalopram-you’re playing with fire. Both St. John’s Wort and SSRIs increase serotonin in the brain. Together, they can trigger serotonin syndrome: a potentially fatal condition with symptoms like high fever, seizures, rapid heartbeat, confusion, and muscle rigidity.
The TGA documented six cases in Australia where people developed serotonin syndrome after combining St. John’s Wort with SSRIs or nefazodone. Symptoms showed up within 3 to 7 days. One patient ended up in intensive care. The risk isn’t theoretical. It’s documented, real, and deadly.
HIV Medications: A Risk You Can’t Afford
If you’re living with HIV, your antiretroviral drugs are your lifeline. Protease inhibitors like saquinavir and ritonavir, and non-nucleoside reverse transcriptase inhibitors like efavirenz, are all metabolized by CYP3A4. St. John’s Wort can slash their blood levels by up to 50%. That means the virus can replicate again. Drug resistance can develop. Treatment fails.
There’s no safe middle ground here. Even a short two-week course of St. John’s Wort can trigger this drop. And because HIV meds need to be taken perfectly every day, any drop in concentration increases the risk of a public health crisis.
Other Dangerous Interactions
- Anticonvulsants: Phenytoin, carbamazepine, and phenobarbital become less effective. Seizures can return. TGA reports cases of breakthrough seizures after St. John’s Wort use.
- Digoxin: Levels drop 25%. This can lead to heart failure worsening in people with atrial fibrillation or heart disease.
- Theophylline: Used for asthma and COPD. Levels drop 30%. Risk of breathing emergencies rises.
- Benzodiazepines: Alprazolam (Xanax) and other anxiety meds lose up to 40% of their effect. Panic attacks return.
- Statins: Atorvastatin and simvastatin drop in effectiveness. Pravastatin and fluvastatin are safer, but you can’t assume all statins are equal.
- Opioids: Some, like oxycodone, may be metabolized faster, reducing pain relief.
- Proton pump inhibitors: Omeprazole and esomeprazole levels can fall, making acid reflux harder to control.

Why People Don’t Realize the Risk
Most people don’t think of herbal supplements as “medications.” They say, “I’m not on any drugs-I just take a little St. John’s Wort.” But here’s the problem: 73% of patients who had dangerous interactions didn’t know they were at risk. And 41% of those taking prescription meds never told their doctor they were using it.
Doctors don’t always ask the right question. Asking “Are you taking any other medications?” misses the mark. People don’t count supplements. You have to ask: “Do you take any herbal products, vitamins, or over-the-counter remedies?” That’s the only way to catch it.
What to Do If You’re Taking St. John’s Wort
If you’re on any prescription drug, stop taking St. John’s Wort-unless your doctor has specifically approved it and is monitoring you. Even then, it’s risky.
If you want to stop using it:
- Don’t quit cold turkey if you’ve been taking it for depression. Talk to your doctor about tapering.
- Wait at least two weeks before starting any new medication that interacts with it. The enzyme-inducing effects linger.
- Get blood tests if you’re on warfarin, cyclosporine, or anticonvulsants. Check levels 3-5 days after stopping St. John’s Wort.
- Use the St. John’s Wort Interaction Checklist from the University of Adelaide. It lists 57 high-risk drugs.
The Bottom Line
St. John’s Wort might help mild depression. Some people swear by it. But the risks aren’t worth it for most people. The American Psychiatric Association no longer recommends it for anyone on prescription meds. The FDA now requires warning labels. Hospitals report dozens of incidents each year. The cost? An average of $18,450 per interaction-because of extra tests, ER visits, and hospitalizations.
There’s no safe dose if you’re on other medications. No “low dose” exception. No “I only took it for a week” loophole. The science is clear: if you’re on a prescription drug, don’t take St. John’s Wort. Period.
If you’re struggling with depression and want to avoid antidepressants, talk to your doctor. There are safer alternatives-therapy, exercise, light therapy, even certain prescription options with fewer interactions. Your health isn’t worth gambling with a supplement that can undo years of medical care.
Can I take St. John’s Wort if I’m not on any medications?
If you’re not taking any prescription drugs, over-the-counter medications, or other supplements, St. John’s Wort may be safe for short-term use in mild depression. But even then, it can cause side effects like dry mouth, dizziness, or increased sun sensitivity. Always check with a healthcare provider before starting any new supplement.
How long does St. John’s Wort stay in your system?
The enzyme-inducing effects of St. John’s Wort can last up to two weeks after you stop taking it. That’s why you need to wait at least 14 days before starting medications like warfarin, cyclosporine, or birth control. The herb doesn’t linger in your blood, but its impact on your liver enzymes does.
Is St. John’s Wort regulated like a drug?
No. In the U.S., it’s sold as a dietary supplement under DSHEA, which means the FDA doesn’t test it for purity, potency, or interactions before it hits shelves. Manufacturers aren’t required to prove it works or is safe with other meds. That’s why labels say, “Ask your doctor before use if you’re taking prescription drugs.”
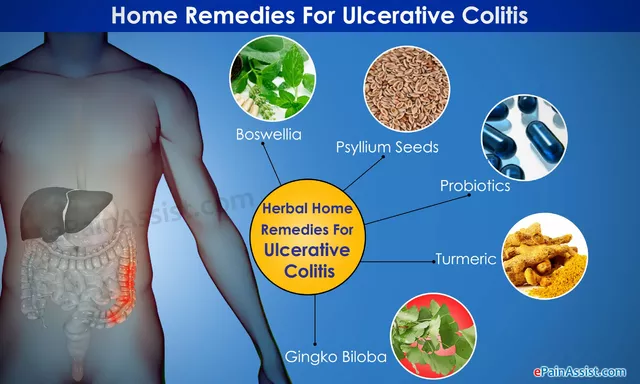
Are there safer herbal alternatives for depression?
There’s no herbal supplement proven to be as effective as prescription antidepressants without risks. Omega-3s, saffron, and curcumin have shown some promise in studies, but none are as well-researched as St. John’s Wort-and none are risk-free. The safest approach is therapy, exercise, sleep hygiene, and, if needed, FDA-approved medications under medical supervision.
What should I tell my pharmacist?
Tell them everything you take-prescriptions, over-the-counter meds, vitamins, and herbal supplements. Pharmacists are trained to spot dangerous interactions. If you don’t mention St. John’s Wort, they can’t warn you. A simple “I take St. John’s Wort for mood” could prevent a hospital visit.
Can I take St. John’s Wort with vitamins or supplements?
Some supplements can add to the risk. For example, combining St. John’s Wort with 5-HTP or L-tryptophan can increase serotonin levels and raise the chance of serotonin syndrome. Even high-dose vitamin B6 may enhance serotonin activity. Stick to basic multivitamins unless your doctor approves anything else.


Tim Goodfellow
18 December 2025 - 11:54 AM
Okay but have you ever seen someone on Reddit try to swap their SSRIs for St. John’s Wort because ‘it’s natural’? I’ve seen it. It’s wild. One guy thought it was like swapping soda for sparkling water. Nope. It’s more like swapping your car’s fuel for battery acid and expecting the engine to run smoother. The liver doesn’t care if it’s ‘herbal’ - it sees a chemical and reacts. This post is basically a public service announcement wrapped in a horror story. Respect.
mark shortus
19 December 2025 - 07:16 AM
OMG I JUST REALIZED I TOOK THIS FOR 3 WEEKS WHILE ON WARFARIN 😭 I THOUGHT IT WAS JUST ‘HERBAL SUPPORT’ LIKE TURMERIC. MY INR WAS FLUCTUATING LIKE A STOCK MARKET CRASH. MY DOCTOR YELLED AT ME. I THOUGHT I WAS BEING HEALTHY. I WAS BEING A WALKING TIKTOK MISTAKE. 🚨💊
Elaine Douglass
19 December 2025 - 18:59 PM
I’m so glad someone finally put this out there. My cousin almost lost her transplant because she thought ‘natural’ meant ‘safe’. She didn’t tell anyone she was taking it. It broke my heart. Please if you’re taking anything else - even just a multivitamin - talk to your pharmacist. They’re the quiet heroes of healthcare.
Takeysha Turnquest
20 December 2025 - 17:40 PM
We live in a world where we worship ‘natural’ like it’s divine truth. But nature doesn’t care if you live or die. Poison ivy is natural. Snake venom is natural. St. John’s Wort? It’s just another molecule with a marketing team. The body doesn’t distinguish between ‘herb’ and ‘pharma’ - only chemistry. And chemistry doesn’t lie. We’re just too emotionally attached to the idea of ‘gentle healing’ to face that.
Vicki Belcher
21 December 2025 - 02:36 AM
This is so important!! 🙏 I used to think supplements were just ‘bonus health’ but now I know they’re like unmarked landmines in your body. My mom takes blood pressure meds and started taking St. John’s Wort for ‘stress’ - I had to gently intervene. She cried. But now she’s safe. 💙 If you’re reading this - please, just ask your doctor. No shame. Just safety.
Aboobakar Muhammedali
22 December 2025 - 12:35 PM
I am from India and here people use this herb for depression all the time. No one knows about interactions. My uncle took it with his heart pills. He ended up in hospital. We thought it was just bad luck. Now I tell everyone. This post saved lives. Thank you.
Laura Hamill
23 December 2025 - 10:24 AM
THE FDA IS IN THE POCKET OF BIG PHARMA. THEY WANT YOU TO TAKE PRESCRIPTIONS. ST. JOHN’S WORT IS A NATURAL CURE THEY’RE SCARED OF. WHY DO YOU THINK THEY PUT WARNINGS ON IT? BECAUSE IT WORKS TOO WELL AND THEY CAN’T PATENT IT. YOU’RE BEING MANIPULATED. DON’T TRUST THE SYSTEM. TRUST NATURE.
Glen Arreglo
24 December 2025 - 15:56 PM
Look, I get the fear. But let’s not demonize herbal medicine either. St. John’s Wort has helped people for centuries - just like aspirin came from willow bark. The issue isn’t the herb, it’s the lack of education. We need better labeling, public awareness, and doctors who actually ask about supplements. This isn’t about fear. It’s about responsibility - from both sides.
shivam seo
24 December 2025 - 16:15 PM
LOL. I’m Australian. We’ve known this since 1998. The TGA reports? We’ve been screaming this for 25 years. Meanwhile, Americans are still buying this stuff like it’s kombucha. Your healthcare system is a joke. Just stop. Read the label. Or don’t. But don’t blame the herb when your blood thinners stop working. You were warned.