SNRI Comparison Tool
Compare SNRI Medications
Select medications to see a comparison
When you’re struggling with depression, anxiety, or chronic pain, finding the right medication can feel like searching for a key that actually fits the lock. SNRIs - serotonin-norepinephrine reuptake inhibitors - are one of those keys for many people. Unlike older antidepressants that only target serotonin, SNRIs work on two neurotransmitters at once: serotonin and norepinephrine. That dual action makes them especially useful when depression comes with fatigue, physical pain, or lack of motivation. But they’re not without trade-offs. Side effects like nausea, high blood pressure, and withdrawal symptoms can be tough to manage. If you’re considering venlafaxine, duloxetine, or another SNRI, here’s what you need to know - straight from real-world use, clinical data, and how these drugs actually behave in the body.
How SNRIs Actually Work (Beyond the Basics)
It’s easy to hear "SNRIs increase serotonin and norepinephrine" and think that’s the whole story. But it’s more nuanced. These drugs block the transporters that pull serotonin and norepinephrine back into nerve cells after they’re released. That leaves more of these chemicals floating in the space between neurons, helping signals get through more clearly. What’s interesting is that not all SNRIs are created equal. Venlafaxine, for example, has a much stronger effect on serotonin than norepinephrine - about 30 times stronger at lower doses. But as the dose goes up, it starts blocking norepinephrine reuptake too. That’s why higher doses (above 150mg/day) are linked to increased blood pressure. Duloxetine and desvenlafaxine are more balanced, but still favor serotonin. Levomilnacipran and milnacipran, on the other hand, tilt toward norepinephrine. That’s why they’re often chosen for pain conditions like fibromyalgia - norepinephrine plays a bigger role in how the body processes pain signals.
There’s also a lesser-known effect: SNRIs can indirectly boost dopamine in the prefrontal cortex. That’s because dopamine and norepinephrine share the same transporter in some brain areas. More norepinephrine blocking means more dopamine sticks around. That might explain why some people feel more alert or focused on SNRIs compared to SSRIs. But it’s not a direct dopamine action - it’s a side effect of the main mechanism. This is why SNRIs aren’t used for ADHD, even though they sometimes help focus. They’re not targeted enough.
Venlafaxine: The Energy Booster With a Catch
Venlafaxine (sold as Effexor XR) was the first SNRI approved in 1993, and it’s still one of the most prescribed antidepressants in the U.S. It’s often chosen when SSRIs like sertraline or escitalopram haven’t worked - especially if the person feels sluggish, unmotivated, or has chronic pain. Many users report a noticeable lift in energy within 2-3 weeks. That’s faster than SSRIs for some. But that energy boost comes with a price.
At doses over 150mg per day, about 12-15% of people develop high blood pressure. That’s why doctors check blood pressure regularly if you’re on higher doses. It’s not a huge risk for most, but if you already have hypertension, venlafaxine might not be the best fit. Another big issue: withdrawal. About 54% of users report what’s called the "venlafaxine cliff" - sudden dizziness, brain zaps, nausea, or anxiety if they miss a dose or stop too fast. That’s because venlafaxine has a short half-life. It leaves your system quickly. That’s why tapering over 4 weeks is standard. Skipping even one day can trigger symptoms.
Side effects? Dry mouth (30% of users), sweating (20%), nausea (25%), and sexual side effects (up to 40%). Many people stop taking it not because it doesn’t work, but because the withdrawal feels worse than the depression.
Duloxetine: The Pain Relief Powerhouse
Duloxetine (Cymbalta, Drizalma Sprinkle) is unique. It’s the only SNRI approved for depression, generalized anxiety disorder, diabetic nerve pain, fibromyalgia, and chronic musculoskeletal pain. That’s rare. Most antidepressants don’t touch pain at all. But duloxetine does - and it works well for it. Studies show it reduces pain scores by 30-50% in people with diabetic neuropathy and fibromyalgia. That’s why it’s often prescribed for people who have both depression and chronic pain. One patient in Austin, who’d been on opioids for years after a back injury, switched to duloxetine and cut her pain meds in half. "It didn’t make me euphoric," she said, "but it made the pain bearable. And I stopped feeling like I was drowning in sadness."
But the trade-off is strong. Nausea hits about 25-30% of users in the first few weeks. For many, it fades after 2-4 weeks. But not everyone. Some drop out because of it. Weight changes are common too - about 37% lose 5-7 pounds early on, then gain it back over months. Sexual side effects are just as common as with venlafaxine: 65% of users report low libido or trouble reaching orgasm. And like venlafaxine, stopping abruptly can cause withdrawal. About 40-50% of people experience dizziness, headaches, or flu-like symptoms if they quit cold turkey.
Other SNRIs: What’s Different?
Desvenlafaxine (Pristiq) is basically the active metabolite of venlafaxine. It’s marketed as having fewer side effects, but studies show it’s about the same. The main difference? It doesn’t need to be titrated - you can start at 50mg. That’s convenient, but doesn’t mean it’s safer. Blood pressure risks are still there.
Levomilnacipran (Fetzima) and milnacipran (Savella) are the norepinephrine-heavy SNRIs. They’re less commonly prescribed because they’re more expensive and have fewer long-term studies. But for people with severe fatigue or pain, they can be a game-changer. Milnacipran is FDA-approved only for fibromyalgia - not depression - so it’s not used as a first-line antidepressant. Levomilnacipran is approved for depression and shows slightly better energy improvement than other SNRIs in trials. But it also carries a higher risk of increased heart rate and blood pressure.
Side Effects You Can’t Ignore
Not all side effects are mild. Here are the big ones:
- Serotonin syndrome: Rare, but dangerous. Happens when SNRIs are mixed with other serotonergic drugs - like tramadol, certain migraine meds, or even St. John’s wort. Symptoms: high fever, confusion, fast heart rate, muscle rigidity. Needs emergency care.
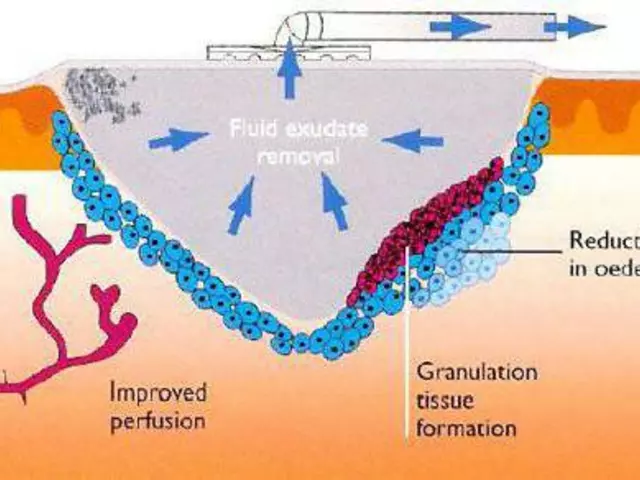
- Bleeding risk: SNRIs reduce serotonin in platelets, which helps blood clot. If you’re on blood thinners or NSAIDs like ibuprofen, your risk of bruising or nosebleeds goes up. Talk to your doctor before combining them.
- Increased blood pressure: Especially with venlafaxine over 150mg/day. Monitor it. If it stays above 140/90, your dose may need adjusting.
- Discontinuation syndrome: Don’t stop suddenly. Even if you feel fine. Taper slowly over 2-4 weeks. Symptoms can last weeks and feel like a bad flu mixed with anxiety.
- Sexual dysfunction: Affects 20-40% of users. Libido drops, arousal slows, orgasm becomes harder. It’s not "all in your head." It’s biological. Some people switch meds. Others add bupropion (an NDRI) to counter it.
And yes - SNRIs can cause weight gain over time. Not because they make you hungry. But because they change how your body uses energy. Some lose weight early, then gain it back. Others gain slowly. It’s unpredictable.
SNRIs vs. SSRIs: When to Choose Which?
SSRIs (like fluoxetine or sertraline) are usually tried first. They’re gentler. Fewer blood pressure issues. Less withdrawal risk. But if you’ve tried one or two and still feel flat, tired, or in pain - SNRIs are the next step.
Here’s a quick guide:
- Choose an SNRI if: You have depression + chronic pain, fatigue, low energy, or didn’t respond to SSRIs.
- Choose an SSRI if: You have anxiety, mild depression, or are sensitive to side effects.
- Avoid SNRIs if: You have uncontrolled high blood pressure, liver disease, or are on MAOIs.
SNRIs aren’t "better." They’re just different. For someone with fibromyalgia and depression, duloxetine might be life-changing. For someone with pure anxiety, an SSRI might be enough - and safer.
What About Tramadol?
Tramadol is an opioid painkiller - but it also blocks serotonin and norepinephrine reuptake. That’s why some people feel a mood lift with it. But it’s not an antidepressant. It’s not approved for depression. And it’s risky. Long-term use can lead to dependence. Seizures are rare but real. And mixing it with SNRIs? That’s a recipe for serotonin syndrome. Don’t combine them unless your doctor specifically says to - and even then, monitor closely.
Practical Tips for Starting an SNRI
If your doctor recommends an SNRI, here’s what to do:
- Start low. Venlafaxine at 37.5mg, duloxetine at 30mg. Don’t rush the dose.
- Expect nausea. Take it with food. It usually fades in 2-4 weeks.
- Track your blood pressure. Especially if you’re on venlafaxine over 150mg.
- Don’t stop suddenly. Even if you feel better. Taper slowly with your doctor.
- Watch for serotonin syndrome. If you start feeling feverish, confused, or your muscles lock up - get help.
- Give it 6-8 weeks. Antidepressants don’t work overnight. Don’t quit too soon.
And remember: SNRIs aren’t magic. They don’t fix trauma, stress, or loneliness. They help your brain function better so you can do the other work - therapy, sleep, movement, connection. That’s the real path to recovery.
What’s Next for SNRIs?
Research is still going. There are 47 active clinical trials looking at SNRIs for PTSD, ADHD, and menopausal hot flashes. One new drug, LY03015, is in Phase III trials and aims for a more balanced serotonin-norepinephrine effect - maybe with fewer side effects. The market for SNRIs is growing, not shrinking. More people are being diagnosed with depression and chronic pain together. And SNRIs are one of the few drugs that treat both.
But the future isn’t just about new pills. It’s about understanding that depression isn’t just a chemical imbalance. It’s inflammation, stress hormones, sleep disruption, and social isolation - all tangled together. SNRIs help untangle part of it. But they’re not the whole solution.
Are SNRIs better than SSRIs for depression?
SNRIs aren’t necessarily "better," but they can be more effective for certain people - especially those with depression plus physical symptoms like fatigue, low energy, or chronic pain. SSRIs are usually tried first because they’re gentler. But if an SSRI doesn’t help after 6-8 weeks, an SNRI is the most common next step. Studies show SNRIs have slightly higher response rates in treatment-resistant depression.
Can SNRIs cause weight gain?
Yes, but it’s complicated. Many people lose a few pounds in the first few weeks due to nausea or reduced appetite. But over 6-12 months, weight gain is common - especially with long-term use. This isn’t true for everyone, but it’s frequent enough that doctors monitor it. The exact reason isn’t clear, but it may involve changes in metabolism and how the body stores fat.
Why do SNRIs cause withdrawal symptoms?
SNRIs change how your brain handles serotonin and norepinephrine. When you stop suddenly, your brain doesn’t have time to readjust. That leads to withdrawal symptoms like dizziness, brain zaps, nausea, and anxiety. Venlafaxine has a short half-life, so it leaves your system fast - making withdrawal worse. Tapering slowly over 2-4 weeks reduces this risk dramatically. Most doctors recommend cutting the dose by 25% every week.
Is it safe to drink alcohol while on SNRIs?
It’s not recommended. Alcohol can worsen side effects like dizziness, drowsiness, and nausea. It can also increase the risk of liver damage, especially with duloxetine. More importantly, alcohol depresses mood - which can counteract the benefits of the medication. Even one drink can make you feel worse. Most doctors advise avoiding alcohol completely when starting an SNRI.
How long does it take for SNRIs to start working?
You might notice small changes in energy or focus within 1-2 weeks. But full antidepressant effects usually take 6-8 weeks. Pain relief from duloxetine or venlafaxine can show up faster - sometimes in 2-4 weeks. Don’t give up if you don’t feel better right away. Patience matters. But if you have severe side effects or suicidal thoughts, contact your doctor immediately.
Can I switch from an SSRI to an SNRI safely?
Yes, but it needs to be done carefully. You can’t just stop one and start the other. Most doctors use a "washout" period - stopping the SSRI for 1-2 weeks before starting the SNRI. This reduces the risk of serotonin syndrome. Some use a cross-taper - slowly reducing the SSRI while slowly increasing the SNRI. Always follow your doctor’s plan. Never switch on your own.
Final Thoughts
SNRIs are powerful tools. They’ve helped millions of people get back their energy, reduce their pain, and find stability. But they’re not perfect. Side effects are real. Withdrawal is common. And they’re not a cure - just a support system while you rebuild your life. If you’re considering one, ask your doctor about your specific symptoms, your health history, and what your goals are. There’s no one-size-fits-all. The right SNRI for you is the one that balances effectiveness with tolerability. And that’s a conversation worth having - not just a prescription to fill.





Sami Sahil
31 January 2026 - 22:39 PM
man i was on venlafaxine for like 8 months and the brain zaps? oh god. felt like my skull was getting electrocuted every time i turned my head too fast. but the energy boost? 10/10. i went from barely getting out of bed to running 5k. just dont stop it cold. i did and it was hell. take it slow, folks. 🙏
Jaden Green
2 February 2026 - 18:12 PM
It is, of course, deeply concerning that the pharmaceutical industry continues to peddle these pharmacologically crude instruments as if they were precision tools. The notion that modulating monoamine reuptake in a non-selective, systemic fashion constitutes "treatment" is a relic of 1970s neurochemistry. We have fMRI, epigenetics, and cytokine profiling now-yet we still prescribe venlafaxine like it’s a vitamin? The reductionist paradigm is not only outdated; it’s ethically indefensible.
Angel Fitzpatrick
2 February 2026 - 21:24 PM
They don't want you to know this but SNRIs are part of the NSA-CIA mind control program. The "brain zaps"? That's not withdrawal-that's the signal from the satellite. They use the short half-life of venlafaxine to keep you hooked because it makes you more suggestible. And the blood pressure spikes? That's how they track your emotional state. They're using your serotonin levels to map dissent. I know this because I read a PDF on a .onion site that had blueprints. Don't take it. Go off-grid. Eat kale. Meditate. They can't control you if you're not plugged in.
Chris & Kara Cutler
3 February 2026 - 13:04 PM
Duloxetine saved my life after my back surgery 😭 no more opioids, no more crying in the shower. Nausea sucked at first but food helped. And yes, sex drive dropped-but I’d rather feel human than horny. 💪
Lisa Rodriguez
4 February 2026 - 22:11 PM
I think it's important to remember that SNRIs aren't the answer for everyone but they can be a bridge. I was on duloxetine for fibromyalgia and yes, the nausea was brutal for the first two weeks but after that? I could actually walk to the mailbox without crying. The key is patience and working with your doctor-not just popping pills and hoping. Also, therapy helped me more than the med ever did. Medication just gave me the energy to show up for it. 🤝
Nicki Aries
5 February 2026 - 17:53 PM
I just want to say-please, please, PLEASE don't stop SNRIs cold turkey. I did. I thought I was fine. I was fine. Until I wasn't. I spent three weeks in a fog of dizziness, electric shocks in my head, and crying for no reason. My doctor said it was "discontinuation syndrome"-I called it "my brain rebelling." Tapering isn't optional. It's survival. And if your doctor says "just cut it in half"-find a new doctor. This isn't a coffee habit. This is neurochemistry. Be gentle with yourself.
Ed Di Cristofaro
7 February 2026 - 12:53 PM
lol people act like these drugs are magic. nah. they're just chemical bandaids. i took venlafaxine for a year. felt like a robot. got off it. life got better. therapy, sleep, walking outside-that's what fixes you. not some pill that makes your hands sweat and your dick not work. stop believing the ads.
Lilliana Lowe
8 February 2026 - 19:26 PM
The assertion that duloxetine reduces pain scores by 30–50% in diabetic neuropathy is misleadingly cited. The actual mean difference in the 2011 Cochrane review was 9.6 points on a 100-point scale, which equates to a 9.6% improvement-not "30–50%" as stated. This is a classic case of relative risk inflation. Furthermore, the phrase "brain zaps" is not a medical term; it is a layperson’s descriptor with no diagnostic validity. Precision in language matters, especially in medical communication.
vivian papadatu
10 February 2026 - 04:24 AM
As someone who grew up in a family where mental health was never talked about, finding out about SNRIs changed everything for me. I didn’t know depression could be physical-like my body felt heavy, like I was underwater. Duloxetine didn’t make me happy, but it let me breathe again. I’m not saying it’s perfect. I had nausea, I had dry mouth, I had to fight to get my libido back. But I’m alive. I’m working. I’m seeing my niece grow up. That’s worth something. And if you’re reading this and you’re scared? Talk to someone. Even if it’s just a Reddit stranger. You’re not alone.