What You Really Need to Know About Nausea Medications in Pregnancy
Over two-thirds of pregnant people experience nausea and vomiting - it’s not just "morning sickness," it’s a real, daily struggle that can make eating, working, or even getting out of bed feel impossible. For about 1 in 10, it gets so bad that hospitalization is needed. The good news? There are safe, effective options. The bad news? Not all meds are created equal. Some carry hidden risks you won’t find on a drug label. Knowing which ones work, which ones are safest, and which ones to avoid could make all the difference in your pregnancy experience.
First-Line Treatments: What Works Without Risk
The American College of Obstetricians and Gynecologists (ACOG) says start with non-drug options before reaching for pills. Ginger is one of the most studied and trusted. Taking 250 mg four times a day - usually as capsules - has been shown in multiple studies to reduce nausea better than a placebo. One 2023 meta-analysis found it cut nausea risk by nearly 80%. Many women report feeling relief within 30 minutes, with no drowsiness or brain fog. The downside? Some say the taste is strong, but capsules bypass that.
When ginger isn’t enough, pyridoxine (vitamin B6) is the next step. Dosing is simple: 25 mg three times a day. It’s not just safe - it’s been used for decades with no link to birth defects. In fact, studies show it works better than placebo at reducing vomiting. Many doctors combine it with doxylamine, an antihistamine found in over-the-counter sleep aids like Unisom. Together, they form Diclegis, the only FDA-approved medication specifically for pregnancy nausea. It’s been on the market since 2013 after being pulled in the 1980s due to legal issues, not safety concerns. Clinical trials confirm it’s effective and safe.
Antacids with calcium carbonate are another underrated first-line tool. If your nausea is tied to heartburn or acid reflux, these can help. Surprisingly, research shows they may even lower the risk of cleft lip or palate (adjusted odds ratio of 0.58). They’re cheap, accessible, and carry zero known fetal risk.
Second-Line Options: When First-Line Isn’t Enough
If you’re still struggling after ginger and B6, antihistamines are the next go-to. Meclizine (Antivert), dimenhydrinate (Dramamine), and diphenhydramine (Benadryl) are all considered safe during pregnancy. Dosing is typically 25-50 mg every 4-6 hours as needed. Studies from the American Academy of Family Physicians show they outperform placebo, with side effects like drowsiness being manageable - especially if you take them at night.
Metoclopramide (Reglan) is another option, used for nausea that comes with slow stomach emptying. It’s not first-line, but it’s been used safely for decades. Some women find it helps with both nausea and vomiting, especially when other meds fail.
One thing to remember: timing matters. Taking meds before symptoms peak - like before breakfast or before getting in the car - works far better than waiting until you’re already sick. Many women wait too long, then wonder why the pill "didn’t work."

The Risky Ones: Ondansetron, Steroids, and PPIs
Ondansetron (Zofran) is the most commonly prescribed medication for severe nausea - and the most controversial. It works. Fast. But it’s not safe for everyone. A major NIH study analyzing over 4,500 pregnancies found a 2.37-fold increase in cerebral palsy risk among babies exposed to ondansetron in the first trimester. That’s not a small risk. It’s not proven to cause it, but the association is strong enough that experts are now urging caution.
Some doctors still prescribe it for hyperemesis gravidarum when nothing else works. But the trend is shifting. More hospitals now require a signed consent form before prescribing it, and many OB-GYNs are moving it to third-line status - only after pyridoxine, doxylamine, and antihistamines have failed.
Proton pump inhibitors (PPIs) like omeprazole are often used for heartburn during pregnancy. But a 2012 NIH study linked them to a startling 4.36-fold increase in hypospadias (a genital birth defect in boys). That’s not something you want to risk if you’re only treating mild reflux. Stick with antacids first. If you need more, talk to your doctor about H2 blockers like famotidine, which have a better safety record.
Corticosteroids like prednisone are sometimes used for extreme, treatment-resistant cases. But they carry a 3.4-fold higher risk of cleft lip or palate when taken in the first trimester. These are not casual options. They’re reserved for hospital settings, and only after every other option has been tried.
What Real Women Are Saying
On Reddit’s pregnancy forum, 78% of over 1,200 women said ginger capsules gave them moderate to complete relief. Many chose them over prescription meds because they didn’t feel groggy. On Amazon, ginger supplements average 4.3 out of 5 stars. The biggest complaint? Taste. But again - capsules solve that.
Users of Diclegis report 84% effectiveness, but 67% say drowsiness is a problem. That’s why most take the doxylamine at night. One user wrote: "I can finally eat breakfast without rushing to the bathroom - but I need a nap by 10 a.m."
Ondansetron reviews tell a different story. In a review pool of over 1,500 users, 32% reported severe side effects: headaches (42%), dizziness (37%), and constipation (29%). Some said the nausea returned worse after the drug wore off.
Acupressure bands? They’re popular, but studies show they’re no better than placebo. One woman on BabyCenter wrote: "I wore those wristbands for weeks. Felt nothing. Felt guilty for wasting $30."
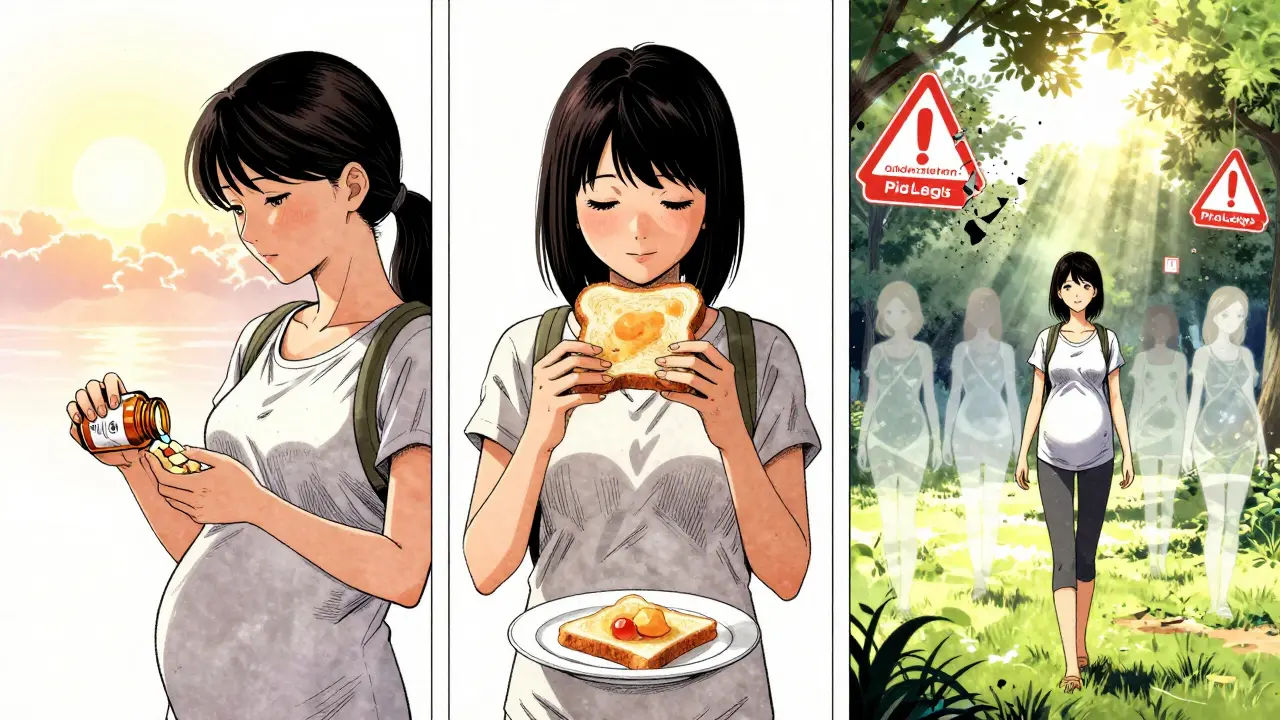
How to Choose - A Simple Decision Path
- Start with ginger (250 mg, 4x/day) - try it for 3-5 days.
- If no improvement, add pyridoxine (25 mg, 3x/day).
- If still struggling, combine pyridoxine with doxylamine (25 mg at bedtime) - this is Diclegis.
- If symptoms persist, ask about antihistamines like meclizine or dimenhydrinate.
- Only consider ondansetron if you’re losing weight, dehydrated, or hospitalized. Get a full risk discussion first.
- Avoid steroids and PPIs unless absolutely necessary and under direct medical supervision.
Don’t wait until you’re vomiting all day. Early treatment prevents complications - including hospitalization. ACOG says the benefits of treating nausea clearly outweigh any theoretical risks. The goal isn’t to eliminate every twinge of nausea. It’s to help you eat, sleep, and function.
What’s Changing in 2025
The FDA is drafting new guidelines for antiemetic safety in pregnancy, with stricter monitoring for drugs used during organogenesis (weeks 3-8). ACOG is updating its 2018 guidelines - expected in mid-2024 - to reflect new data on ondansetron and PPIs. Hospitals like Mayo Clinic and Cleveland Clinic have already cut hyperemesis hospitalizations by over 30% using standardized protocols that start with ginger and B6.
Meanwhile, the ginger supplement market is booming - it makes up 73% of all complementary medicine sales for pregnancy nausea. That’s not marketing. That’s women choosing what works - and what’s safest.
Pyridoxine and doxylamine will remain the gold standard. Ginger will stay the top natural choice. Ondansetron? Its days as a go-to are ending. The evidence is too clear.
Bottom Line: You Have Control
You don’t have to suffer. You don’t have to guess. You don’t have to take the first pill your doctor suggests. Ask about ginger. Ask about B6. Ask about timing. Ask about risks. If your provider dismisses you, find one who listens. Nausea in pregnancy isn’t "just part of it." It’s a medical issue with real solutions - and real risks if you choose poorly.
Start simple. Stay informed. Prioritize safety. Your body is doing something incredible - don’t let nausea steal your peace of mind.
Is ginger safe during pregnancy?
Yes, ginger is considered safe during pregnancy and is recommended by ACOG as a first-line treatment. Studies show 250 mg taken four times daily reduces nausea without increasing the risk of birth defects. It’s been used for decades with no evidence of harm to the fetus.
Is Diclegis safe for my baby?
Yes. Diclegis is the only FDA-approved medication specifically for nausea in pregnancy. It combines pyridoxine (vitamin B6) and doxylamine, both of which have decades of safety data. No link to birth defects has been found at standard doses. It’s considered the safest oral option available.
Why is ondansetron (Zofran) risky in pregnancy?
A large NIH study found a 2.37-fold increase in cerebral palsy risk among babies exposed to ondansetron in the first trimester. While the absolute risk is still low, the association is strong enough that experts now recommend avoiding it unless other treatments have failed and hospitalization is needed. Many doctors now reserve it for extreme cases only.
Can I take antacids while pregnant?
Yes, antacids containing calcium carbonate are not only safe - they may reduce the risk of cleft lip or palate. They’re ideal for nausea tied to heartburn. Avoid antacids with aluminum or magnesium if you have kidney issues. Stick to calcium-based options like Tums.
What if nothing works?
If you’re losing weight, dehydrated, or can’t keep anything down for more than 24 hours, contact your provider immediately. You may need IV fluids and stronger treatments like metoclopramide or, in rare cases, hospital-based care. Don’t wait until you’re exhausted. Early intervention prevents serious complications.
Are acupressure wristbands worth it?
No. Multiple studies, including a 2023 meta-analysis, show acupressure bands have the same effect as placebo. They’re not harmful, but they won’t reliably reduce nausea. Save your money and focus on proven options like ginger, B6, or Diclegis.
Should I stop prenatal vitamins if they make me sick?
If iron is making you nauseous, ask your doctor about switching to an iron-free prenatal for the first trimester. You can add iron later when nausea improves. Taking your vitamin at night with food, or switching to a gummy form, can also help. Don’t stop without talking to your provider - folic acid is critical in early pregnancy.






Jerry Peterson
20 December 2025 - 19:12 PM
Ginger capsules changed my life in the first trimester. No drowsiness, no weird side effects. Just felt like I could breathe again. Took them before breakfast and suddenly food didn’t feel like a threat.
Wish I’d known this sooner.
Adrian Thompson
22 December 2025 - 04:03 AM
They say ginger is safe but who’s really funding these studies? Big Pharma wants you to think natural = useless so they can sell you Diclegis for $500 a month. Wake up. The FDA’s been compromised since 2008. They banned thalidomide but let Zofran through? Coincidence? I think not.
Jon Paramore
24 December 2025 - 04:00 AM
The 2.37x cerebral palsy risk with ondansetron is real but needs context: absolute risk is still under 1%. That said, if you’ve got access to B6 + doxylamine and it’s working? Don’t gamble. Metoclopramide’s got a better safety profile than Zofran if you need something stronger than OTCs. Timing matters - take meds 30 min before nausea peaks, not after.
Swapneel Mehta
26 December 2025 - 01:52 AM
I’m from India and we’ve used ginger and cardamom for nausea for generations. It’s funny how modern medicine is just catching up. The science backs it. The wisdom was always there. Maybe we don’t need to reinvent the wheel every time.
Cameron Hoover
26 December 2025 - 10:55 AM
I almost lost my job because I couldn’t keep anything down. Then I tried the B6 + Unisom combo. It wasn’t magic - but it was enough. I could sit through meetings. I could eat a banana. I could cry without feeling like a failure. This isn’t just about nausea. It’s about dignity.
Stacey Smith
27 December 2025 - 08:12 AM
Zofran is a scam. My OB pushed it like it was aspirin. I asked for alternatives. She said 'you’re lucky you even have options.' I left and found a midwife who actually listened. Ginger, B6, and sleep. That’s it. No pills. No guilt.
Michael Ochieng
27 December 2025 - 10:01 AM
I’m a dad. My wife went through hell with HG. We tried everything. Ginger didn’t work for her. Diclegis made her sleep 12 hours a day. But she ate. She kept weight on. We didn’t end up in the hospital. That’s the win. Safety isn’t about zero side effects. It’s about keeping you alive and sane.
Erika Putri Aldana
29 December 2025 - 01:54 AM
Why are we even talking about this like it’s a medical decision? It’s a corporate one. Companies make billions off pregnancy nausea. Ginger? Can’t patent it. Diclegis? Patent protected. Zofran? Off-label = profit. Wake up. The system doesn’t care if you’re sick. It cares if you’re buying.
Grace Rehman
30 December 2025 - 03:53 AM
We treat nausea like a flaw in the system instead of a signal. What if your body is telling you something? Maybe it’s not about suppressing it but understanding it. That said - if you can’t eat, sleep, or function - then yes, meds are valid. Not because you’re weak. Because you’re human.
Siobhan K.
31 December 2025 - 22:56 PM
The PPI-hypospadias link is real but often misinterpreted. 4.36x sounds scary until you realize baseline risk is 0.03%. So it becomes 0.13%. Still low. But if you have mild reflux? Stick with Tums. If you’re on PPIs long-term for GERD? Talk to your doc about switching to famotidine. Risk isn’t binary - it’s a spectrum.
Meina Taiwo
2 January 2026 - 14:46 PM
In Nigeria, we use lime and salt water. Works surprisingly well. No pills needed. But if you’re in the US and have access to science-backed options? Use them. Don’t feel guilty. Your health matters too.
Southern NH Pagan Pride
3 January 2026 - 22:28 PM
they say ginger is safe but what about the heavy metals in the capsules? and who tests the supplements? the fda doesn’t regulate them like drugs. so you’re trusting some chinese factory that says ‘natural’ on the bottle. i’d rather take the zofran than risk lead poisoning.
Orlando Marquez Jr
4 January 2026 - 10:50 AM
The evidence base for first-line interventions is robust and methodologically sound. The meta-analyses referenced demonstrate statistically significant efficacy with minimal adverse event profiles. The shift in clinical guidelines reflects a maturation of obstetric pharmacovigilance, not ideological bias.
Jackie Be
5 January 2026 - 13:11 PM
I took Zofran and it saved me from hospitalization. Don’t hate on it because you had a good experience with ginger. Some of us are in crisis mode. I cried in the ER because I hadn’t eaten in 72 hours. Don’t shame people who need help.
John Hay
6 January 2026 - 12:55 PM
This post is exactly what I needed. I was about to ask my doctor for Zofran. Now I’m going to start with ginger and B6. If it doesn’t work, I’ll come back. No guilt. No rush. Just smart choices.