After a stroke, your body is in a fragile state. The risk of another stroke is highest in the first year-and that’s where high-dose statins come in. But are they helping you, or just adding new problems? This isn’t just about lowering cholesterol. It’s about balancing a real chance to prevent another stroke against real risks like muscle pain, liver stress, and even bleeding in the brain.
Why High-Dose Statins Are Used After Stroke
Most strokes are caused by blocked arteries due to plaque buildup. Statins work by blocking an enzyme called HMG-CoA reductase, which your liver uses to make cholesterol. High-dose statins-usually atorvastatin 80 mg daily-can drop LDL ("bad") cholesterol by 50% or more. That’s much more than moderate doses, which typically lower it by 30-40%.
The landmark SPARCL trial in 2006 followed over 4,700 people who’d recently had a stroke or TIA. Those on high-dose atorvastatin had a 16% lower risk of another stroke over nearly five years. That might sound small, but in real numbers: out of 100 people, 13 would have another stroke on placebo, but only 11 would on high-dose statin. That’s 2 fewer strokes per 100 people. Multiply that across millions of stroke survivors, and it adds up.
But here’s the catch: this benefit only shows up in people with atherosclerotic stroke-where plaque clogs brain arteries. If your stroke came from a heart rhythm problem like atrial fibrillation, statins don’t help much. That’s why doctors don’t just hand out high-dose statins to everyone after stroke. They look at the cause.
The Hidden Risks: More Than Just Muscle Pain
When people hear "statin side effects," they think of muscle aches. And yes, about 5-10% of users report this. But high-dose statins carry heavier risks.
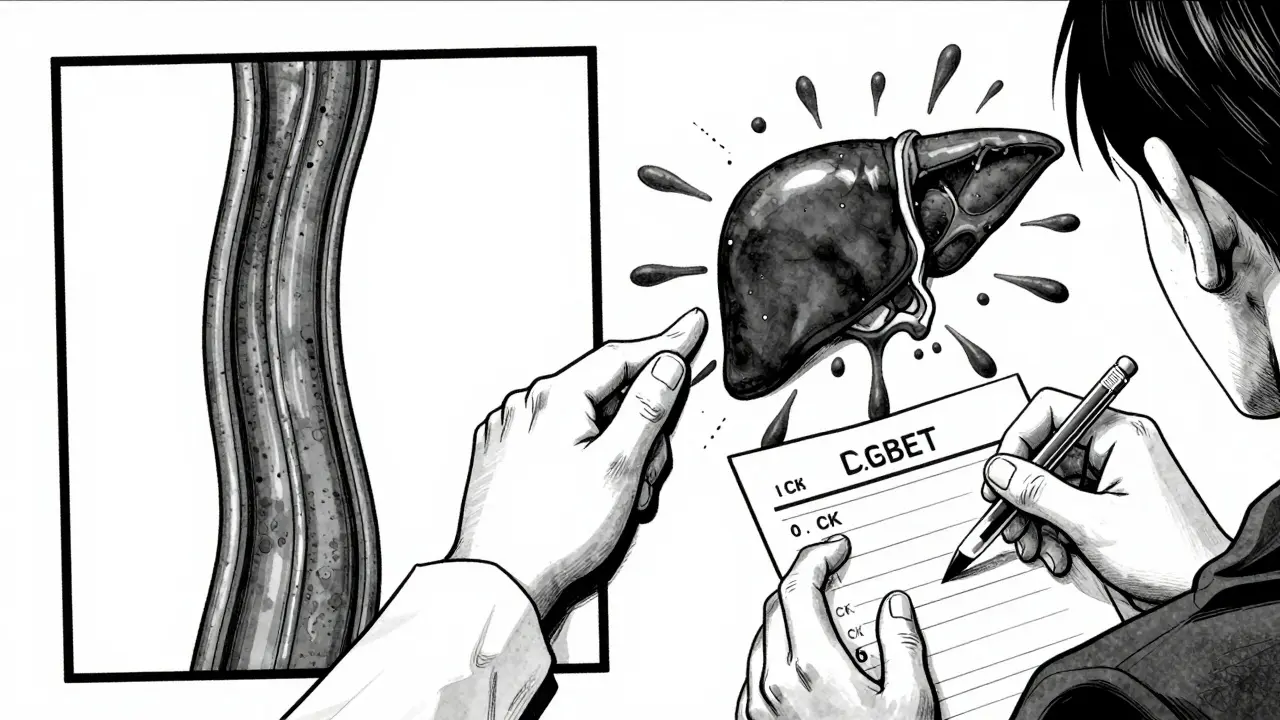
One major concern is liver enzyme spikes. In the SPARCL trial, 1.2% of people on atorvastatin 80 mg had persistent liver enzyme elevations-compared to just 0.2% on placebo. That doesn’t mean liver damage, but it does mean your doctor needs to check your liver function every 3-6 months.
Even more troubling: hemorrhagic stroke risk. The same SPARCL trial found that high-dose statins increased the chance of bleeding in the brain from 1.4% to 2.3%. That’s nearly double. This isn’t theoretical. A 2022 meta-analysis confirmed that higher statin doses correlate with higher hemorrhagic stroke risk. For someone who already had a hemorrhagic stroke, or has high blood pressure or brain vessel abnormalities, this could be dangerous.
And then there’s the issue of muscle damage. Simvastatin 80 mg was pulled from the market in 2011 after the FDA warned about severe muscle breakdown (rhabdomyolysis), especially when taken with common blood pressure drugs like amlodipine. Atorvastatin is safer in that regard, but it’s still not risk-free.
Who Benefits Most-and Who Should Be Careful
Not everyone needs high-dose statins after stroke. Your doctor should consider:
- Stroke type: Atherosclerotic stroke? High-dose statin likely helps. Cardiac embolism? Probably not.
- History of bleeding: If you’ve had a brain bleed before, or have uncontrolled high blood pressure, statins might do more harm than good.
- Age and frailty: Older adults, especially those over 75, are more prone to side effects. Lower doses often work just as well for prevention.
- Other medications: Drugs like amiodarone, cyclosporine, or strong antifungals can spike statin levels in your blood. This raises muscle and liver risks.
There’s also a surprising group: people without diabetes or high cholesterol. A 2024 study in JAMA Neurology found that these patients actually had the biggest benefit from early, high-dose statin therapy. It’s not just about cholesterol levels-it’s about stabilizing plaque and reducing inflammation in the arteries.
Real-World Problems: Why People Stop Taking Them
Here’s the ugly truth: many people stop taking statins after stroke. The REGARDS study found that only 48.7% of stroke patients were even prescribed statins when they left the hospital. And among those who were, nearly one in three quit within six months.
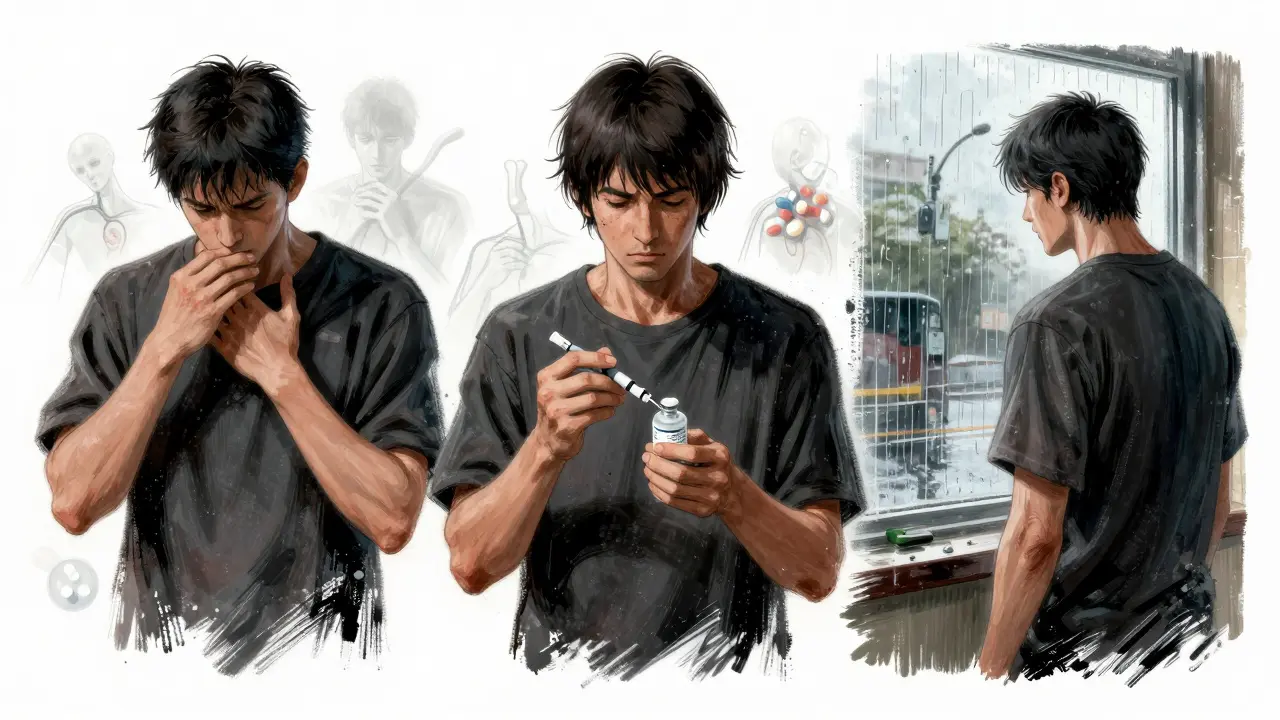
Why? Muscle pain tops the list. But so do digestive issues, fatigue, and the vague feeling of "brain fog." Some patients think, "I feel fine now, why keep taking a pill with side effects?"
But stopping statins is risky. A 2023 study showed patients who quit within six months had a 42% higher chance of having another stroke. That’s not a small number. It’s not just about cholesterol-it’s about the protective effects on blood vessels.
And here’s the good news: you don’t have to quit. If side effects hit, talk to your doctor. Switching from atorvastatin 80 mg to 40 mg often keeps the benefit while cutting side effects. Switching to rosuvastatin or pravastatin can help too. Some people even do every-other-day dosing. The goal isn’t perfection-it’s staying on some form of therapy.
What’s New in 2025: Science Is Evolving
The old idea-"more statin is always better"-is fading. A 2024 study tested giving high-dose statins within 72 hours of stroke. It didn’t reduce stroke risk in the next 90 days, though it slightly improved recovery. That suggests timing matters less than we thought.
Meanwhile, a new trial called STROKE-STATIN is underway. It’s tracking 1,200 patients to see if starting statins immediately after stroke improves long-term function. Results are expected in late 2024.
And then there’s the rise of alternatives. PCSK9 inhibitors like evolocumab and alirocumab lower LDL even more than statins-without increasing bleeding risk. But they’re expensive, need injections, and aren’t first-line yet. For now, they’re mostly for patients who can’t tolerate statins or have had a hemorrhagic stroke.
What Should You Do?
If you’ve had a stroke and are on high-dose statins:
- Don’t stop without talking to your doctor.
- Ask: "Is this helping prevent another stroke, or just lowering my cholesterol?"
- Request a liver enzyme and CK blood test every 3-6 months.
- If you have muscle pain, ask about switching to a different statin or lowering the dose.
- Make sure your blood pressure is under control-this matters more than statin dose for preventing brain bleeds.
If you’re not on statins after stroke:
- Ask your neurologist or cardiologist why not.
- Find out what type of stroke you had. If it was atherosclerotic, statins are likely recommended.
- Ask about moderate-dose statins if high-dose feels too risky.
The bottom line: high-dose statins after stroke aren’t magic. They’re a tool. A powerful one-but one that can backfire if used carelessly. The goal isn’t to take the highest dose possible. It’s to take the right dose for you.
Are high-dose statins safe after a stroke?
High-dose statins can be safe for many stroke survivors, especially those with atherosclerotic stroke. But they carry risks, including increased chances of brain bleeding, liver enzyme changes, and muscle pain. Safety depends on your stroke type, other health conditions, and medications. Always monitor with blood tests and talk to your doctor before making changes.
Do statins increase the risk of another stroke?
Statins reduce the risk of another ischemic stroke (caused by clots) by about 20%. But they may slightly increase the risk of hemorrhagic stroke (caused by bleeding) in some people, especially at high doses. This is why doctors carefully weigh your stroke type and risk factors before prescribing.
Can I switch to a lower dose if I have side effects?
Yes. In fact, this is often the best move. Studies show that reducing the dose-like going from atorvastatin 80 mg to 40 mg-still provides most of the stroke-prevention benefit while cutting side effects. Never stop cold turkey. Talk to your doctor about switching statins or lowering the dose.
Why do some stroke patients stop taking statins?
Common reasons include muscle pain, fatigue, digestive issues, or believing they "feel fine" now. But stopping statins increases the risk of another stroke by up to 42% within six months. Many patients who quit later regret it. If side effects occur, work with your doctor to adjust the dose or type-not quit entirely.
Are there alternatives to high-dose statins after stroke?
Yes. For patients who can’t tolerate statins or have a history of brain bleeding, PCSK9 inhibitors (like evolocumab) are an option. They lower LDL more than statins without increasing bleeding risk. But they’re expensive and require injections. For most people, moderate-dose statins remain the best balance of safety and effectiveness.




Charlotte Dacre
14 February 2026 - 16:55 PM
So let me get this straight - we’re giving people who just had a stroke a drug that can cause brain bleeds... and calling it 'prevention'? The logic here is thicker than atorvastatin sludge. I mean, if I had a leaky pipe, I wouldn’t pour more water on it and call it plumbing. But hey, Big Pharma’s got a nice ROI, I guess. 🤷♀️
Mike Hammer
14 February 2026 - 18:19 PM
i took atorvastatin for like 3 months after my tia and honestly? felt like a zombie. muscle pain, brain fog, just... drained. switched to 40mg and life improved. no one told me i could drop the dose. they just said 'take it or risk another stroke.' well, i risked it and still here. maybe the system needs to stop treating patients like robots.
Kaye Alcaraz
15 February 2026 - 18:46 PM
It is imperative that stroke survivors understand that medication adherence is not optional-it is foundational to long-term recovery. While side effects are valid concerns, discontinuation without medical supervision significantly elevates recurrence risk. A collaborative dialogue with your healthcare provider can yield personalized adjustments that preserve efficacy while minimizing adverse events. Your health is worth the effort.
Chiruvella Pardha Krishna
16 February 2026 - 02:12 AM
The human body is not a machine to be calibrated with chemical levers. Statins suppress cholesterol because we have been taught that cholesterol is the villain. But what if the real villain is inflammation? What if the real solution lies not in blocking enzymes but in healing the vessel walls? We treat symptoms, not causes. And so we cycle-stroke, statin, side effect, repeat. The truth is buried under clinical trials and corporate brochures.
Josiah Demara
16 February 2026 - 06:58 AM
The SPARCL trial? Please. 16% relative risk reduction sounds impressive until you realize it’s 2 fewer strokes per 100 people over 5 years. That’s not medicine-that’s statistical theater. And now we’re telling people to take 80mg daily because some paper says so? Meanwhile, 30% of patients quit because they’re not dumb. They feel the cost. The real scandal? We don’t test for plaque stability. We just shove statins down throats like vitamins.
Mandeep Singh
17 February 2026 - 22:58 PM
You people are so naive. You think muscle pain is the worst? Try having your liver enzymes spike and your doctor shrug and say 'it’s normal.' I had a 72-year-old patient on 80mg who developed rhabdomyolysis because he was also on amiodarone. No one checked interactions. No one asked about diet. Just 'take the pill.' And now he’s on dialysis. This isn’t healthcare. It’s a numbers game. Statins are not the answer. The answer is stopping the overprescribing culture before someone dies because someone didn’t read the footnote.
Esha Pathak
19 February 2026 - 02:30 AM
Statins after stroke? 🤔 It’s like giving a drowning man a life jacket made of lead. You’re trying to save him… but the weight might sink him. I mean, we’ve all been told cholesterol is the enemy. But what if the real enemy is stress? Sleep? Sugar? Or maybe… we’re just too obsessed with pills and forget about walking, breathing, and eating real food? 🌱💧 Maybe the real magic isn’t in the bottle… it’s in the garden. 🌿
Daniel Dover
20 February 2026 - 09:34 AM
Lower dose works. Switched from 80 to 40. LDL still under 70. No muscle pain. No liver issues. My neurologist agreed. Simple.
Erica Banatao Darilag
21 February 2026 - 13:28 PM
i just wanted to say thank you for writing this. i had a stroke last year and was put on 80mg atorvastatin. i had terrible fatigue and muscle cramps. i was scared to say anything because i thought i was being weak. but after reading this, i talked to my doctor and we switched to rosuvastatin 10mg. i feel 80% better. i didn’t know it was okay to ask for adjustments. thank you for normalizing that.
Joe Grushkin
23 February 2026 - 08:29 AM
The fact that you're even debating this is why medicine is broken. If you're not on high-dose statins after a stroke, you're not being aggressively managed. You're not being treated-you're being babysat. The data is clear. The risks are manageable. The alternative? A second stroke. That's not a 'choice.' That's negligence wrapped in a 'personalized medicine' bow. Stop romanticizing side effects. Save lives. Take the pill.