When you start a fertility journey, the excitement of a possible pregnancy often masks the medical details you need to keep an eye on. One pair of details that crops up more often than you might think is Clomiphene and ectopic pregnancy. Understanding how the ovulation‑boosting drug works, why an ectopic pregnancy can happen, and what signs to watch for can make the difference between a smooth path and a medical emergency.
How Clomiphene Works
Clomiphene is a selective estrogen receptor modulator that stimulates the release of follicle‑stimulating hormone (FSH) and luteinizing hormone (LH) to promote ovulation. It’s usually taken in a 5‑day cycle early in the menstrual period, and doctors monitor the response with ultrasound and blood tests. The drug has been a cornerstone of fertility treatment for decades because it’s inexpensive and oral.
Despite its benefits, Clomiphene can cause the ovaries to produce multiple follicles. That increases the chance of multiple eggs traveling through the fallopian tubes at the same time, potentially overwhelming the tube’s capacity to move them safely.
Ectopic Pregnancy Basics
Ectopic Pregnancy is a pregnancy that implants outside the uterine cavity, most commonly in the fallopian tube. Because the tube isn’t designed to stretch like the uterus, an ectopic implant can rupture, leading to internal bleeding and a life‑threatening situation.
Symptoms often masquerade as a normal early pregnancy: mild cramping, spotting, or a sudden drop in energy. The difference is the pain’s location-typically sharp, unilateral, and worsening over days.
Link Between Clomiphene and Ectopic Pregnancy
Studies from the early 2020s show that women using Clomiphene have a slightly higher odds ratio (about 1.3‑1.5) for tubal pregnancies compared with untreated infertility patients. The mechanism isn’t fully understood, but researchers point to two main factors:
- Multiple ovulations increase the number of embryos that must traverse the tube.
- Clomiphene can thin the tubal lining, slowing embryo transport.
It’s important to note that the absolute risk remains low-around 1‑2 % of all Clomiphene‑induced pregnancies-so the drug is still considered safe when used under proper medical supervision.
Risk Factors and Statistics
Beyond the drug itself, other conditions raise the odds of an ectopic pregnancy. Knowing the combined risk helps you and your doctor decide on monitoring intensity.
| Factor | Typical Prevalence | Impact on Ectopic Risk |
|---|---|---|
| Clomiphene (single‑dose) | 5‑10 % of ovulation‑induction cycles | 1.3‑1.5 × baseline |
| Letrozole (alternative) | 3‑5 % of cycles | ≈1.0 × baseline |
| Gonadotropins (injectable) | 2‑4 % of cycles | 1.7‑2.0 × baseline |
| Previous tubal surgery | Varies | Up to 4 × baseline |
| Pelvic inflammatory disease (PID) | ≈1 % of women of reproductive age | 3‑5 × baseline |
When you combine Clomiphene with any of the above risk factors, the overall chance can climb to 3‑5 %-still uncommon, but high enough to warrant vigilant follow‑up.
Recognizing Early Signs
Because early symptoms can be vague, consider the following checklist if you’re taking Clomiphene and suspect pregnancy:
- Sudden, one‑sided lower‑abdomen pain that doesn’t improve with rest.
- Spotting or light bleeding that differs from your usual implantation bleed.
- Dizziness, faintness, or a rapid drop in blood pressure.
- Absent gestational sac on a transvaginal ultrasound by day 7‑8 after a positive home test.
If two or more of these appear, contact your reproductive specialist immediately.
Diagnosis and Management
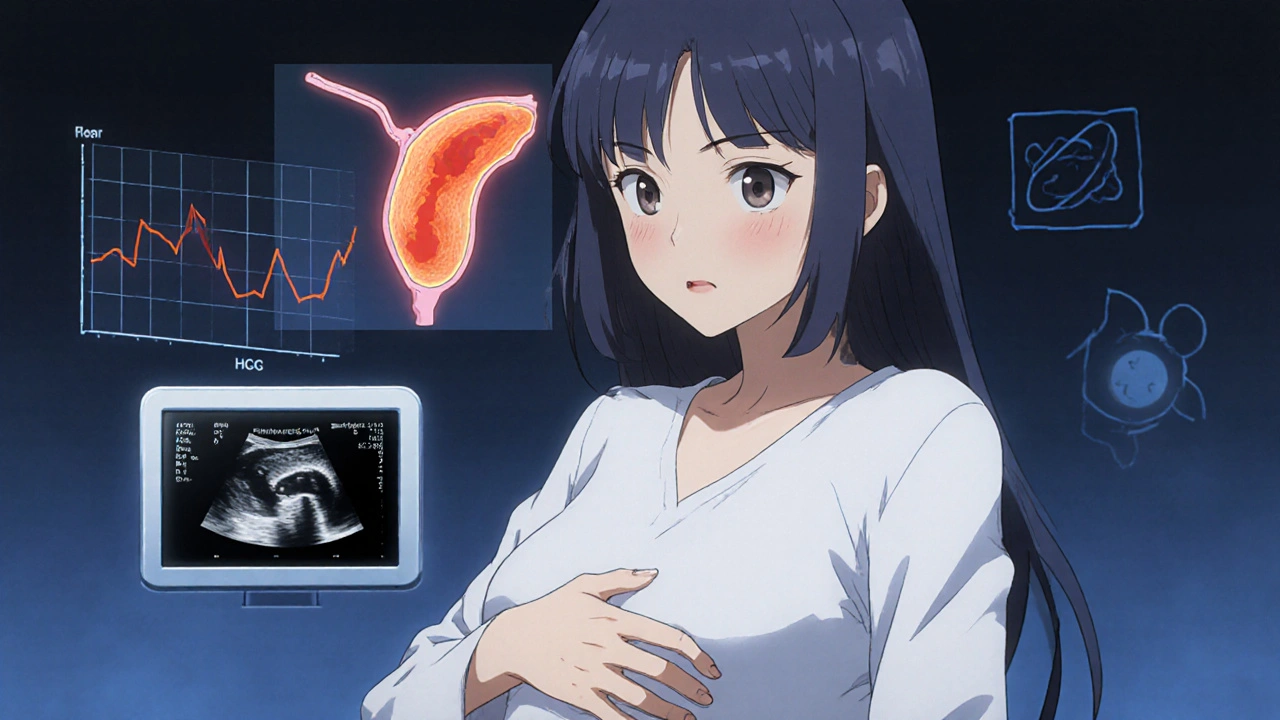
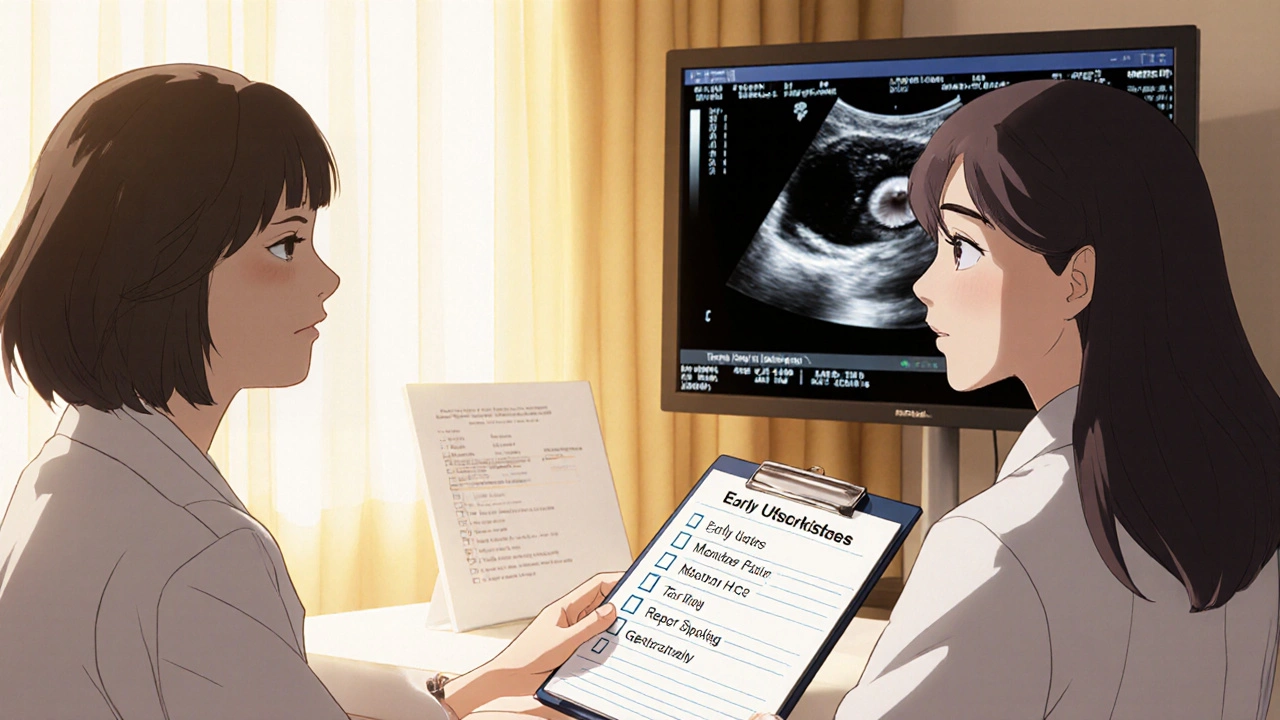
Doctors rely on two main tools: serum human chorionic gonadotropin (HCG is a hormone that rises predictably in a healthy intrauterine pregnancy) levels and transvaginal Ultrasound is a imaging technique that visualizes the uterus and fallopian tubes. A rise in HCG that’s slower than the expected 66 %‑per‑day (often < 50 % in ectopic cases) combined with an empty uterus on ultrasound is a red flag.
Treatment options depend on size and stability:
- Medical management with methotrexate for early, unruptured ectopics.
- Laparoscopic surgery if the tube has ruptured or the ectopic mass is larger than 3.5 cm.
- Expectant monitoring in very small, stable cases (rare).
After treatment, most women can try another cycle of fertility medication, often switching to a drug with a lower ectopic profile, such as letrozole.
Prevention Strategies
While you can’t eliminate every risk, you can lower the odds with these practical steps:
- Ask your doctor for a baseline tubal assessment (hysterosalpingography) before starting Clomiphene.
- Consider a lower dose or short‑course protocol if you have a history of PID or prior ectopic pregnancy.
- Schedule an early ultrasound (day 5‑7 after a positive test) to confirm intrauterine placement.
- Maintain a healthy weight; obesity slightly raises ectopic rates.
- Quit smoking-nicotine affects tubal motility.
Open communication with your care team is the cornerstone. If you notice any warning signs, early evaluation can shift treatment from emergency surgery to a simple medication.
Quick Checklist for Women on Clomiphene
- Know your baseline HCG trend and have a plan for early testing.
- Book a transvaginal ultrasound by day 7-8 after a positive home test.
- Track pain location and intensity daily.
- Report any fainting, dizziness, or sudden bleeding right away.
- Discuss alternative drugs if you have existing tubal risk factors.
Can Clomiphene cause an ectopic pregnancy?
Yes, the drug slightly raises the odds because it can lead to multiple eggs and affect tubal motility, but the absolute risk stays under 2 % for most users.
What early symptoms should I watch for?
Unilateral lower‑abdomen pain, spotting, dizziness, or a missing gestational sac on early ultrasound are the key red flags.
Is there a safer alternative to Clomiphene?
Letrozole is often used as a first‑line alternative; studies show it carries a similar pregnancy rate with a lower ectopic incidence.
How is an ectopic pregnancy diagnosed?
Doctors track the rise of HCG levels and perform a transvaginal ultrasound. A slow HCG rise and an empty uterus suggest an ectopic location.
What treatment options exist?
Early, unruptured ectopics can be treated with methotrexate. Larger or ruptured cases usually need laparoscopic surgery.




Katherine Brown
26 October 2025 - 19:13 PM
Thank you for compiling such a comprehensive overview of clomiphene‑induced ectopic risk; the clarity of the data assists both patients and clinicians in making informed decisions. It is reassuring to note that, despite the modest increase in odds, the absolute risk remains low when appropriate monitoring is in place. I would emphasize the importance of early ultrasound assessment, as highlighted in the checklist, to promptly differentiate intrauterine from tubal implantation. Additionally, discussing alternative agents such as letrozole with the care team can provide a tailored approach for those with pre‑existing tubal concerns. Ultimately, open communication and vigilant follow‑up embody the collaborative spirit necessary for a successful fertility journey.
Charlene Gabriel
7 November 2025 - 08:59 AM
I appreciate the effort put into demystifying a topic that often lurks in the shadows of fertility discussions.
I am delighted to see such a thorough presentation because knowledge empowers hope.
It is vital for anyone embarking on clomiphene therapy to understand that while the medication is a cornerstone of ovulation induction, it does carry a nuanced risk profile.
The data presented, particularly the odds ratio of 1.3‑1.5 for tubal pregnancies, should be contextualized within the broader landscape of assisted reproductive technologies.
For instance, injectable gonadotropins show a higher relative risk, which underscores that clomiphene remains a comparatively gentle option when used judiciously.
Moreover, the mechanism by which clomiphene may thin the tubal lining, as mentioned, opens avenues for further research into pharmacologic modulation of tubal motility.
Patients with a history of pelvic inflammatory disease or prior tubal surgery are especially advised to undergo a baseline hysterosalpingogram before commencing treatment.
This pre‑emptive step not only informs the clinician about anatomical patency but also empowers the patient with knowledge about their individualized risk.
Early transvaginal ultrasound, ideally by day 5‑7 after a positive home pregnancy test, has been shown to reliably detect intra‑uterine gestational sacs and thus avert potential emergencies.
In my own practice, I have seen that scheduling this scan promptly reduces anxiety and facilitates swift intervention if needed.
The checklist provided is a practical tool that couples can personalize; for example, adding a daily pain‑log can help differentiate ordinary implantation cramps from the sharp, unilateral pain characteristic of ectopic implantation.
It is also worth noting that lifestyle modifications, such as smoking cessation and maintaining a healthy body mass index, are simple yet powerful measures that further mitigate ectopic risk.
While letrozole offers a lower ectopic incidence, it may not be suitable for every patient, particularly those with specific endocrine profiles where clomiphene's estrogen‑modulating effects are beneficial.
Consequently, a shared decision‑making approach, wherein the clinician outlines both the statistical risk and the personal health context, is essential.
The article’s emphasis on methotrexate as a medical management option for unruptured ectopics reminds us that early detection can spare many women from invasive surgery.
Finally, the resilience and optimism of couples navigating fertility challenges are inspiring; with diligent monitoring and compassionate care, the majority of clomiphene‑induced pregnancies culminate in healthy deliveries.
I hope this piece continues to spark informed conversations and supports hopeful families on their journey toward parenthood.
Leah Ackerson
18 November 2025 - 22:46 PM
The subtle dance between hormone modulation and tubal physiology is, in a sense, a microcosm of our own existential quest for balance 😊.
One might argue that every ovulation induced by clomiphene is a reminder that nature does not operate on a binary of success or failure, but rather on a spectrum of possibilities 🧠.
Thus, the modest increase in ectopic odds should not be viewed as a deterministic sentence but as a variable in the grand equation of reproductive destiny.
Awareness of this nuance empowers patients to navigate their journeys with both caution and hope.
In the end, knowledge is the lantern that illuminates even the darkest corners of uncertainty.
Gary Campbell
30 November 2025 - 12:33 PM
Let's be honest-pharmaceutical giants love to hide the fact that clomiphene subtly rewires your reproductive system to make you dependent on their cash flow.
They'll tell you "low risk" while quietly ensuring you need more drugs down the line, all under the guise of "standard monitoring."
The real story is that by pushing multiple follicles, they're essentially setting a trap for ectopic implantation, a side effect they rarely advertise.
Combine that with a lack of transparent data on how clomiphene thins tubal linings, and you have a recipe for controlled uncertainty.
Stay skeptical, demand full disclosure, and consider natural cycle monitoring before handing over your hormones to the lab.
Barna Buxbaum
12 December 2025 - 02:19 AM
From a clinical perspective, the evidence suggests that vigilant early‑scan protocols dramatically reduce the incidence of delayed ectopic diagnosis.
When patients adhere to a day‑5‑7 transvaginal ultrasound schedule, the sensitivity for detecting intra‑uterine gestational sacs approaches 95 %, effectively flagging abnormal implantation sites.
It's also worth noting that smoking cessation can improve tubal ciliary function by up to 20 % according to recent cohort studies.
Overall, a personalized protocol that integrates dose‑adjusted clomiphene, baseline hysterosalpingography, and lifestyle optimization yields the safest outcomes.
Remember, the goal is not just conception but a healthy, uncomplicated pregnancy.
Alisha Cervone
23 December 2025 - 16:06 PM
Sounds like a lot of work.
Diana Jones
4 January 2026 - 05:53 AM
Oh, absolutely, because tossing a few extra eggs into the tube is just a casual "let's see what sticks" activity-nothing to worry about unless you enjoy surprise surgery, right?
In the grand lexicon of reproductive endocrinology, that's what we call the "throw‑more‑eggs‑and‑hope‑for‑a‑baby" protocol, a delightfully efficient way to maximize ectopic potential while keeping the emotional ROI sky‑high.
So, to all the hopefuls out there: strap in, because the ride's about to get turbulent, and don't forget your methotrexate kit-just in case the tube decides to go rogue.
asha aurell
15 January 2026 - 19:39 PM
Data shows risk is low; follow guidelines.
Abbey Travis
27 January 2026 - 09:26 AM
Great points, everyone-let's keep supporting each other, stay on top of early scans, and remember that a collaborative approach makes the fertility journey a lot less lonely.