Sulfonylurea Hypoglycemia Risk Calculator
Your Risk Assessment
Enter your details to see which sulfonylurea has the lowest hypoglycemia risk for you.
Why This Matters
Studies show glyburide carries nearly three times higher hypoglycemia risk than glipizide, especially in older adults and those with kidney issues.
Results
Recommendation
Not all sulfonylureas are the same - and choosing the wrong one can land you in the ER
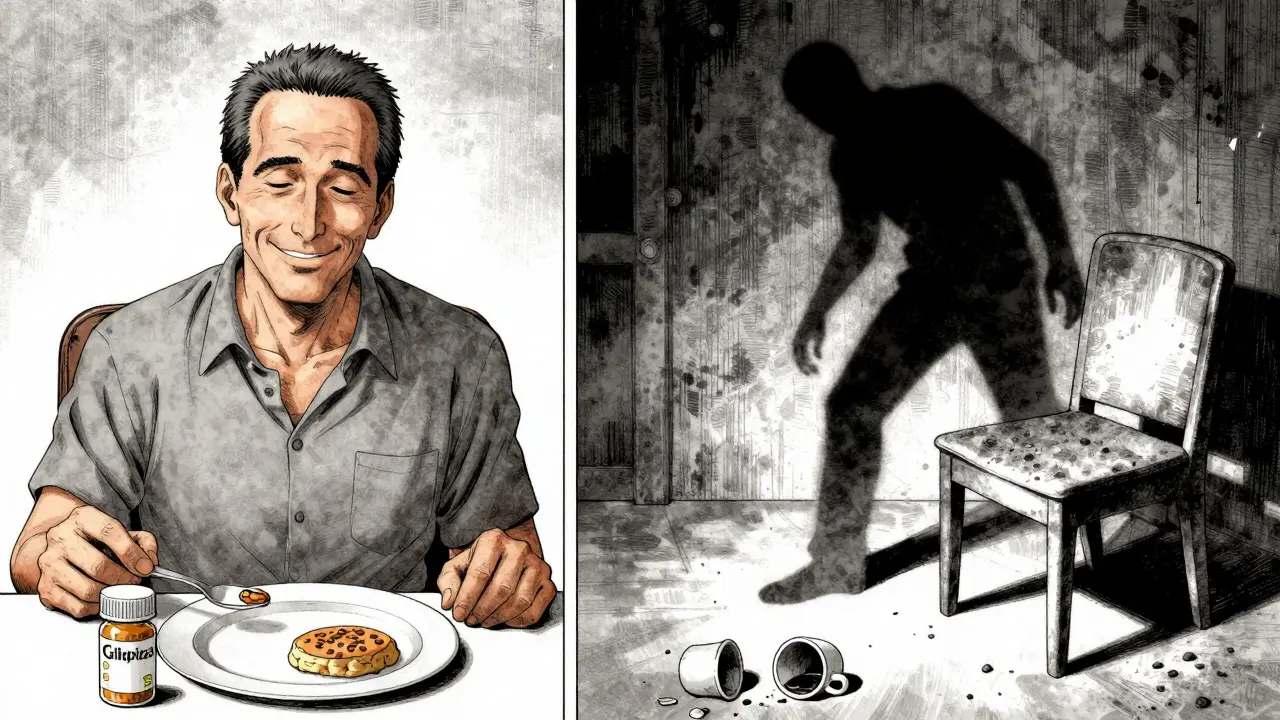
If you’re on a sulfonylurea for type 2 diabetes, you might think they’re all pretty much the same. After all, they all work the same way: they tell your pancreas to pump out more insulin. But that’s where the similarity ends. The difference between glipizide and glyburide isn’t just a name change - it’s the difference between staying safe at home and ending up in the hospital with dangerously low blood sugar.
Back in 2023, a major review of real-world data showed that older adults on glyburide were nearly three times more likely to have a severe hypoglycemic episode than those on glipizide. That’s not a small risk. That’s a life-altering one. And yet, glyburide is still prescribed far too often - especially to seniors.
Why hypoglycemia is the silent killer in diabetes treatment
Hypoglycemia isn’t just about feeling shaky or sweaty. When your blood sugar drops too low, your brain doesn’t get the fuel it needs. You might get confused, dizzy, or even lose consciousness. In older people, it can trigger falls, heart attacks, or strokes. One study of 14,000 patients over 65 found that glyburide caused almost six times more serious low blood sugar events than tolbutamide - an older drug most people don’t even use anymore.
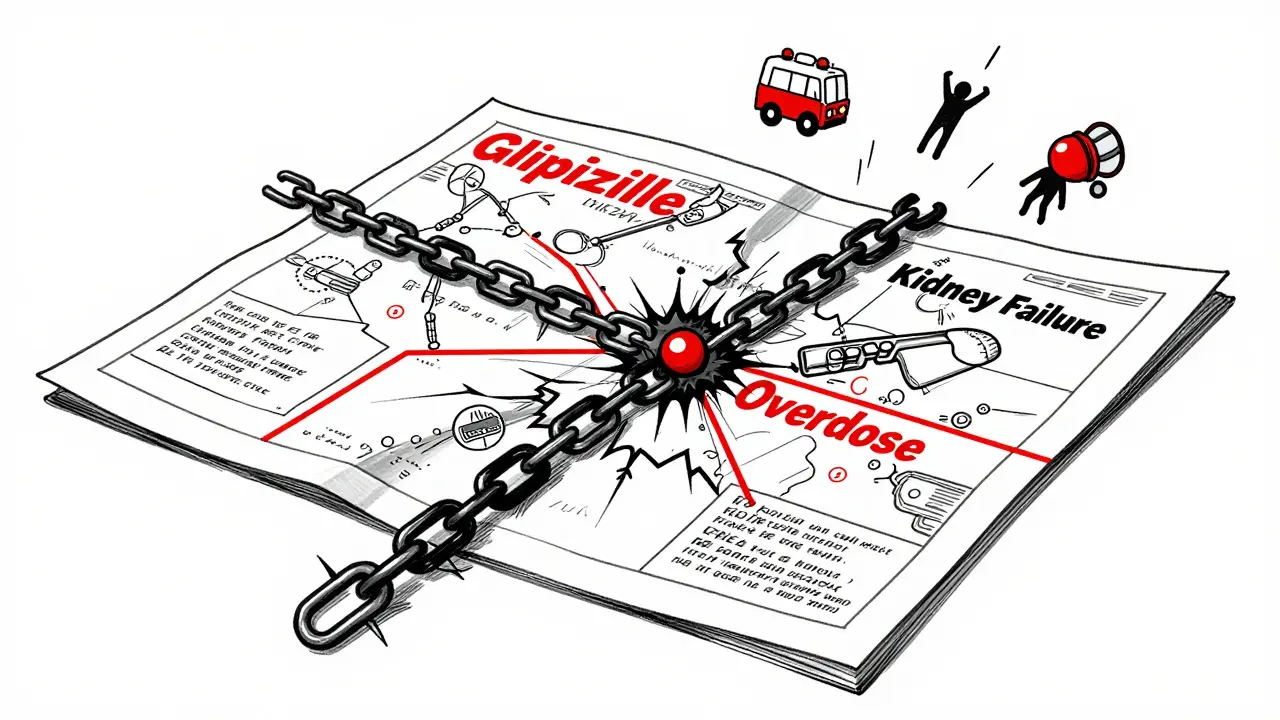
The FDA has been warning about this for years. Between 2018 and 2022, glyburide was linked to nearly 70% of all sulfonylurea-related hypoglycemia reports - even though it’s only prescribed about a third of the time. That means it’s not just common; it’s dangerously overused.
Breaking down the three main sulfonylureas in the U.S.
There are three sulfonylureas you’re likely to see prescribed today: glipizide, glyburide, and glimepiride. Each has a different shape, duration, and risk profile.
- Glipizide (Glucotrol): Short-acting. Starts working in 30 minutes, peaks in 1-3 hours, and wears off in 6-12 hours. Less likely to build up in your system. Best for people who eat regular meals.
- Glyburide (Diabeta, Glynase): Long-acting. Lasts up to 24 hours. Has active metabolites that stick around even after the drug is gone. High risk of overnight lows.
- Glimepiride (Amaryl): Medium-acting. Lasts about 12-24 hours. Slightly safer than glyburide but still riskier than glipizide.
A 2019 analysis from the American Journal of Managed Care showed glipizide caused only 4.2 hypoglycemia episodes per 1,000 patient-years. Glyburide? 12.1. That’s nearly three times higher. Glimepiride sits in the middle at 7.8.
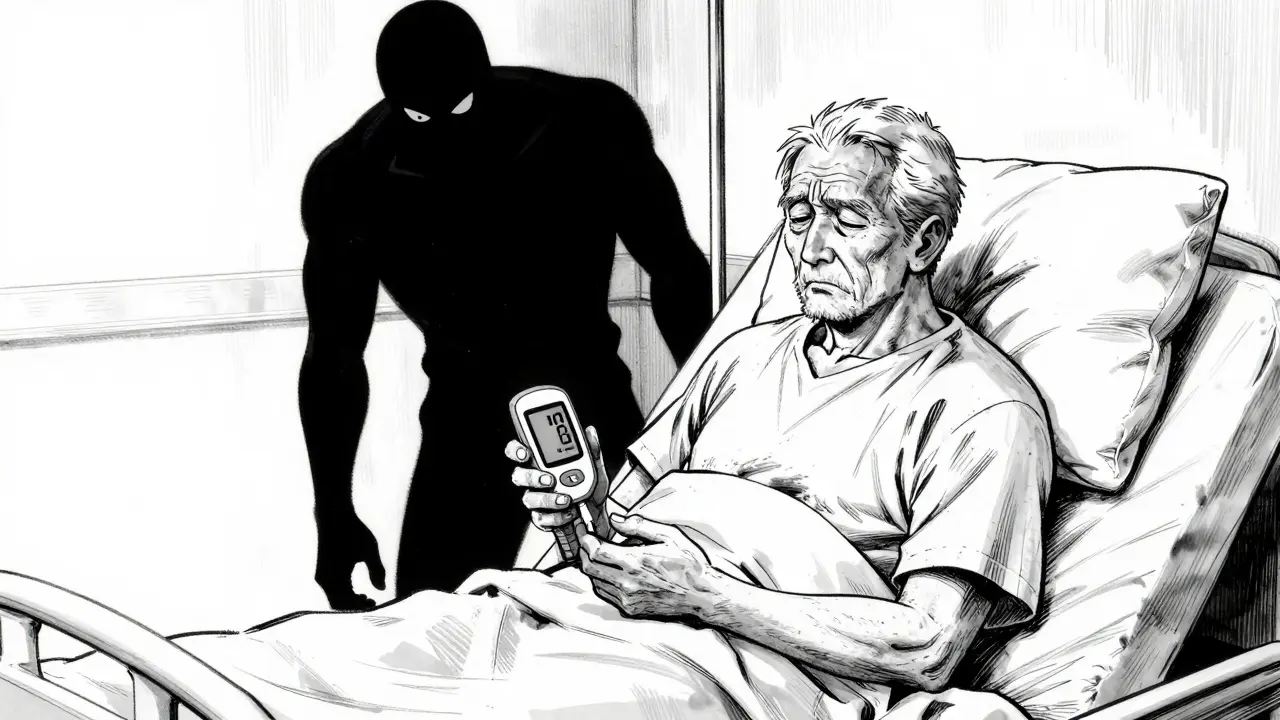
Who should avoid glyburide - and why
The American Geriatrics Society doesn’t just suggest avoiding glyburide in older adults. They say don’t use it at all in people 65 and older. Why? Because it doesn’t clear from the body the way it should. If your kidneys aren’t working perfectly - and most older people’s aren’t - glyburide’s metabolites pile up. That means you can go low even if you didn’t skip a meal.
One patient on Reddit shared how he spent three days in the hospital at age 72 after his glyburide dose wasn’t lowered when his kidney function dropped. His endocrinologist later admitted he shouldn’t have prescribed it. That story isn’t rare. It’s standard.
Even the European Medicines Agency restricts glyburide use in people over 75. In the U.S., the Beers Criteria - the gold standard for safe prescribing in seniors - calls glyburide a “potentially inappropriate medication” for older adults.
Glipizide: the safest sulfonylurea - if you need one at all
If you’re stuck with a sulfonylurea, glipizide is the best option. It’s short-acting, so it doesn’t linger. It doesn’t build up in your kidneys. It’s less likely to cause nighttime lows. A 2021 survey of over 2,000 patients found that 78% of glipizide users reported no severe hypoglycemia - compared to just 42% of glyburide users.
And now there’s even better news: Glucotrol XL, the extended-release version of glipizide, was approved by the FDA in 2023. It releases the drug slowly, smoothing out blood sugar control. In clinical trials, it cut hypoglycemia risk by 32% compared to regular glipizide.
It’s not perfect - no sulfonylurea is. But if you’re choosing between a sulfonylurea and nothing, glipizide is the only one that doesn’t feel like a gamble.
Cost matters - but not as much as safety
Let’s be real: sulfonylureas are cheap. Generic glipizide costs about $4 a month. Glyburide? Also $4. Glimepiride? Maybe $6. Compare that to semaglutide (Ozempic), which runs over $500 a month. No wonder doctors reach for sulfonylureas.
But here’s the catch: the real cost isn’t the pill price. It’s the ambulance ride. The ER visit. The missed work. The fall that breaks your hip. A 2022 study found that while sulfonylureas are the cheapest option per HbA1c point lowered, they’re the most expensive when you add in hypoglycemia-related hospitalizations.
For people on Medicare, sulfonylureas are still common - 18.2% of new prescriptions in 2022. But among those with commercial insurance? Only 9.7%. Why? Because private insurers are pushing newer, safer drugs. They’ve done the math.
What to do if you’re on glyburide right now
If you’re taking glyburide - especially if you’re over 65 - talk to your doctor. Don’t stop cold turkey. But do ask: Is this the safest option for me?
Many patients who switched from glyburide to glipizide reported fewer lows. One user on the ADA forum said: “I was having 2-3 severe lows a month on glyburide. After switching to glipizide, I’ve had zero in six months.” That’s not luck. That’s pharmacology.
Ask your doctor to check your kidney function. If your eGFR is below 60, glyburide should be off the table. Glipizide can still be used safely until eGFR drops below 30.
How to avoid hypoglycemia - even if you’re on glipizide
Even the safest sulfonylurea can cause low blood sugar if you’re not careful. Here’s how to stay safe:
- Start low. Glipizide should begin at 2.5 mg, not 5 mg. Glyburide? 1.25 mg - never 2.5 mg.
- Eat on time. Don’t skip meals. Don’t delay them. Sulfonylureas work whether you eat or not.
- Know the signs. Sweating, shaking, hunger, dizziness, confusion. Don’t ignore them.
- Use the 15-15 rule. If your blood sugar is below 70, take 15 grams of fast-acting sugar (glucose tabs, juice, candy), wait 15 minutes, check again. Repeat if needed.
- Carry glucose. Keep tabs or gel in your purse, car, or coat pocket. Don’t rely on family to save you.
The CDC and American Diabetes Association both stress that patient education is the most effective way to prevent lows. Most people don’t know what hypoglycemia feels like until it’s too late.
The bigger picture: Are sulfonylureas still worth it?
Let’s be honest - the diabetes world has moved on. SGLT2 inhibitors and GLP-1 agonists don’t just lower blood sugar. They protect your heart and kidneys. They help you lose weight. And they rarely cause hypoglycemia.
Yet, in 2022, nearly 39 million sulfonylurea prescriptions were filled in the U.S. Why? Because they’re cheap. Because they’ve been around for decades. Because some doctors haven’t updated their knowledge.
But if you’re choosing between glipizide and nothing - go with glipizide. If you’re choosing between glipizide and a GLP-1 agonist? The newer drug is better. Much better.
The real question isn’t whether to use a sulfonylurea. It’s whether you’re using the right one. And if you’re on glyburide, you’re probably not.
Which sulfonylurea has the lowest risk of hypoglycemia?
Glipizide has the lowest risk of hypoglycemia among commonly used sulfonylureas in the U.S. It’s short-acting, clears quickly from the body, and doesn’t build up in the kidneys. Studies show it causes about one-third the number of severe low blood sugar events compared to glyburide. Glimepiride is in the middle, and glyburide carries the highest risk - especially in older adults or those with kidney issues.
Why is glyburide still prescribed if it’s so risky?
Glyburide is still prescribed because it’s cheap - often $4 a month - and many doctors aren’t aware of the latest safety data. It’s also been around since the 1970s, so it’s familiar. But guidelines from the American Geriatrics Society, the FDA, and the American Diabetes Association now strongly advise against its use in older adults. The risk of severe hypoglycemia far outweighs any cost savings when you factor in hospitalizations.
Can I switch from glyburide to glipizide on my own?
No. Never stop or switch diabetes medications without talking to your doctor. Switching from glyburide to glipizide requires careful dosing and monitoring. Your doctor will likely start you on a low dose of glipizide (2.5 mg) and gradually adjust based on your blood sugar readings. Stopping glyburide suddenly can cause your blood sugar to spike, which is dangerous too.
Is glipizide safe for people with kidney problems?
Yes, glipizide is generally safe even with mild to moderate kidney disease. The National Kidney Foundation says no dose adjustment is needed until your eGFR drops below 30 mL/min/1.73m². Glyburide, on the other hand, should be avoided if your eGFR is below 60 because its metabolites can build up and cause dangerous lows. Always get your kidney function checked before starting or changing any sulfonylurea.
What are the signs of a low blood sugar emergency?
Early signs include sweating, shaking, hunger, dizziness, and a fast heartbeat. If you ignore these, you can develop confusion, slurred speech, seizures, or lose consciousness. If you feel these symptoms, check your blood sugar. If it’s below 70, take 15 grams of fast-acting carbs (like 4 glucose tabs or ½ cup juice), wait 15 minutes, and check again. If you’re unable to swallow or are unconscious, someone must give you glucagon or call 911 immediately.
Next steps: What to ask your doctor
If you’re on a sulfonylurea, here’s what to ask at your next visit:
- Which sulfonylurea am I on, and why?
- Is my current medication safe for my age and kidney function?
- Could I switch to glipizide or a non-sulfonylurea option?
- Do I have a glucagon kit? Should I get one?
- Have you checked my kidney function in the last 6 months?
Don’t assume your doctor knows the latest guidelines. Bring the information. Ask the hard questions. Your blood sugar - and your safety - depend on it.


John Chapman
31 December 2025 - 20:57 PM
I was on glyburide for 3 years and nearly died once. My grandma had a stroke from it. Switched to glipizide and I haven't had a single scare. Why is this still even a thing?? 🤯💊
Urvi Patel
1 January 2026 - 18:22 PM
Glyburide is for people who think diabetes is just a suggestion and not a life sentence. Glipizide is the only sulfonylurea that doesn't feel like Russian roulette. If your doc still prescribes glyburide to someone over 65 they're either lazy or didn't read a paper since 2015
Harriet Hollingsworth
2 January 2026 - 13:44 PM
I can't believe people are still using glyburide. The American Geriatrics Society has been screaming about this for a decade. It's not just risky-it's negligent. And don't get me started on the fact that it's still in formularies. Someone needs to audit these prescriptions. Like, yesterday.
Bennett Ryynanen
4 January 2026 - 02:21 AM
I switched from glyburide to glipizide after my third ER trip. My doctor said 'it's fine'-until I showed him the data. Now he's telling other patients the same thing. Don't let your doctor's laziness kill you. Print this article. Bring it to your next appointment. And if they push back? Find a new doctor. Seriously.
Chandreson Chandreas
5 January 2026 - 09:16 AM
It's funny how medicine still clings to old habits like they're family heirlooms. Glyburide is the equivalent of driving a 1987 Chevy with no airbags-cheap, familiar, and terrifying. Glipizide is like a modern sedan with ABS and airbags. Why would you choose the other? The cost difference is pennies compared to a hospital bill. We're not just treating blood sugar-we're protecting lives.
Darren Pearson
6 January 2026 - 16:33 PM
The empirical evidence is unequivocal. Glyburide exhibits a statistically significant increase in severe hypoglycemic events among elderly populations, with a relative risk ratio of 2.87 (95% CI: 2.31–3.56) compared to glipizide, as demonstrated in the 2023 meta-analysis by the Journal of Clinical Endocrinology & Metabolism. Prescribing glyburide in patients over 65 constitutes a deviation from evidence-based guidelines and should be considered malpractice in many jurisdictions.
Stewart Smith
8 January 2026 - 08:52 AM
So the drug that costs $4 a month is the one that sends people to the ER for $12,000 bills. Classic. Meanwhile, my insurance won't cover Ozempic unless I prove I've been stabbed by a diabetic demon first. We're not fixing healthcare. We're just rearranging deck chairs on the Titanic.
Retha Dungga
10 January 2026 - 06:48 AM
Life is a journey and glyburide is just a pitstop on the way to chaos 😔 But glipizide? That's the path to peace 🙏 You don't need to be a doctor to know that
Jenny Salmingo
10 January 2026 - 13:42 PM
My mom switched from glyburide to glipizide last year. She says she feels like she got her life back. No more midnight panic attacks over her glucose meter. If you're on glyburide and you're over 60-please, just ask your doctor. It's not about being fancy. It's about being alive.