SSRI Bleeding Risk Calculator
Assess Your Bleeding Risk
This tool calculates your bleeding risk based on your SSRI medication, concurrent medications, and health factors. Results are for informational purposes only - always consult your doctor for medical advice.
Your Risk Assessment
Enter your information above to see your risk assessment.
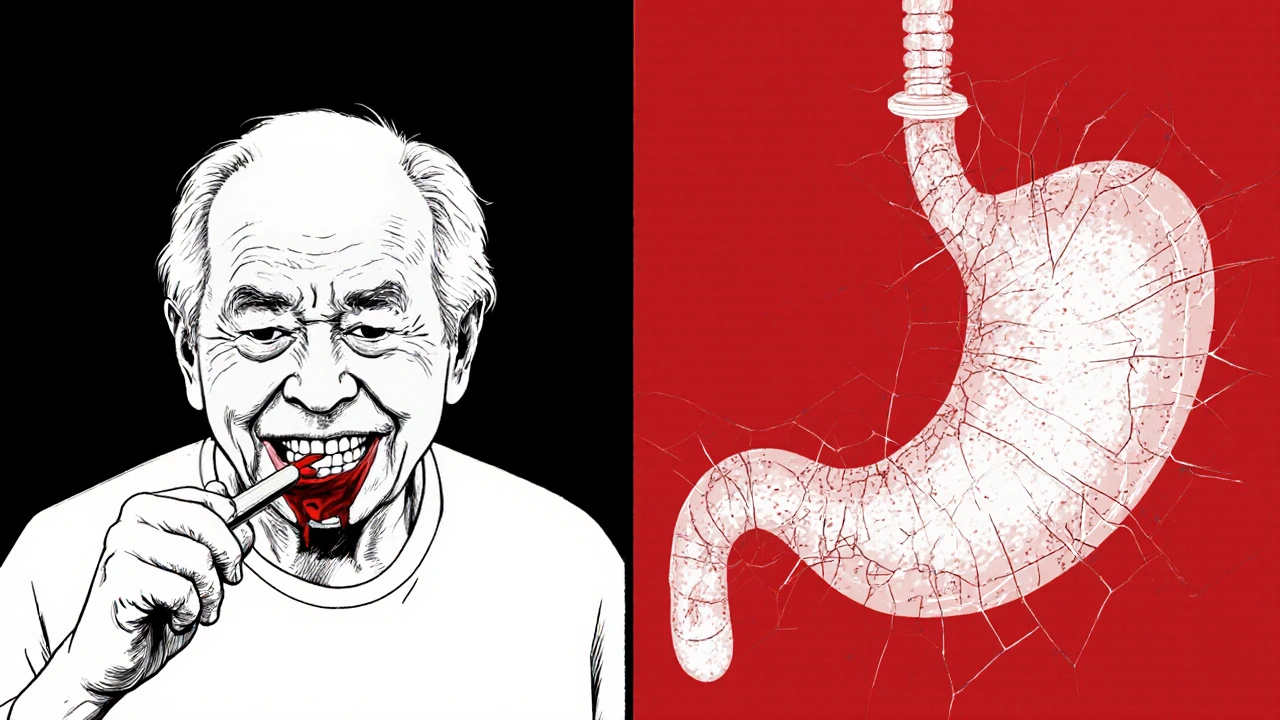
When you take an SSRI for depression or anxiety, you’re not just changing your mood-you’re also changing how your blood clots. It’s not something most people think about, but the same mechanism that lifts your spirits can also make you bleed more easily. If you’ve noticed unexplained bruising, longer bleeding from cuts, or nosebleeds that won’t stop, it might not be bad luck. It could be your antidepressant.
How SSRIs Disrupt Your Platelets
SSRIs like sertraline, fluoxetine, and paroxetine work by blocking the reuptake of serotonin in the brain. That extra serotonin helps improve mood. But here’s the catch: 99% of your body’s serotonin isn’t in your brain-it’s in your platelets. These tiny blood cells rely on serotonin to stick together and form clots when you get hurt. When SSRIs block the serotonin transporter on platelets, they drain away that serotonin. Without it, platelets can’t activate properly. They become sluggish. They don’t clump like they should.Studies show that people taking paroxetine, one of the strongest SSRIs at blocking serotonin uptake, lose more than 80% of their platelet serotonin. That’s not a small drop. It’s enough to seriously mess with your body’s ability to stop bleeding. Even if your blood looks normal on a standard lab test, your platelets might be working at half speed.
Not All SSRIs Are the Same
If you’re worried about bleeding, not all SSRIs carry the same risk. It comes down to how tightly each drug binds to the serotonin transporter. The tighter the grip, the more it disrupts platelets.Paroxetine and fluvoxamine are the worst offenders. Their binding strength (Ki values under 0.4 nM) means they shut down serotonin uptake almost completely. That’s why paroxetine users have a 40-50% higher chance of stomach bleeding compared to people on other antidepressants. Sertraline and citalopram? They’re weaker binders. Their Ki values are higher, meaning they leave more serotonin in the platelets. That’s why sertraline is often the go-to choice for patients with bleeding risks.
Here’s a quick breakdown:
| SSRI | Binding Affinity (Ki) | Bleeding Risk Level | Common Side Effect: Easy Bruising |
|---|---|---|---|
| Paroxetine | 0.17 nM | High | 18.7% |
| Fluvoxamine | 0.34 nM | High | 16.2% |
| Fluoxetine | 0.45 nM | Moderate | 11.8% |
| Sertraline | 0.52 nM | Low-Moderate | 9.2% |
| Citalopram | 0.91 nM | Low | 8.5% |
These numbers aren’t just lab data. Real people report them. On patient forums, 74% of users who noticed easy bruising were on paroxetine. Only 32% of those on sertraline had the same issue. That’s a big difference.
The Big Danger: Mixing SSRIs with Other Drugs
The real problem isn’t usually SSRIs alone. It’s when they’re stacked on top of other blood-thinning meds.If you’re taking warfarin, apixaban, or rivaroxaban (anticoagulants), your risk of major bleeding jumps by 35%. That’s not a small increase. It’s the difference between a minor nosebleed and a dangerous gastrointestinal bleed. Combine SSRIs with NSAIDs like ibuprofen or naproxen? Your bleeding risk goes up 4.5 times. That’s because NSAIDs hurt the stomach lining, and SSRIs stop your platelets from fixing the damage.
Even over-the-counter painkillers can be risky. A lot of people don’t realize that taking Advil for a headache while on an SSRI could be dangerous. The same goes for aspirin-even low-dose aspirin for heart protection can add up with SSRIs. Doctors often miss this combo because they focus on the heart condition and forget the antidepressant.
Who’s at Highest Risk?
Not everyone on SSRIs bleeds. But some people are sitting on a ticking clock.- People over 65
- Those with a history of ulcers or GI bleeding
- Patients with kidney or liver disease
- Anyone on blood thinners or antiplatelet drugs like clopidogrel
- People scheduled for surgery or dental work
The HAS-BLED score is a tool doctors use to measure this risk. It looks at things like high blood pressure, past bleeding, and lab results. If your score is 3 or higher, you’re in the high-risk zone. That’s when switching to a safer SSRI-or even a different type of antidepressant like bupropion or mirtazapine-makes sense.
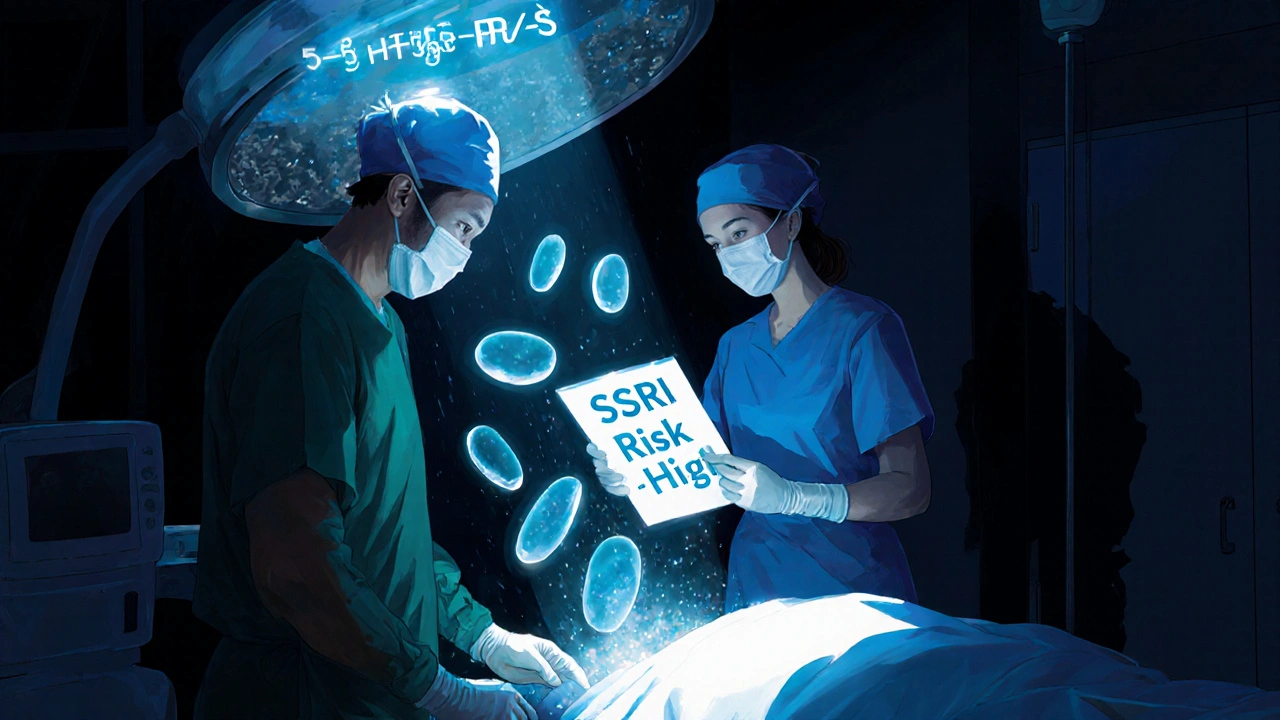
What Happens During Surgery?
This is where things get tricky. Some doctors will tell you to stop your SSRI a week before surgery. Others say keep taking it. Why the conflict?For heart surgery, the American Psychiatric Association says: keep the SSRI. Stopping it can trigger severe depression or even suicidal thoughts-risks that often outweigh bleeding concerns. But for a colonoscopy, a tooth extraction, or a knee replacement? That’s different. For minor procedures with bleeding risk, stopping the SSRI for 5-7 days can cut your chances of complications.
Here’s the catch: platelets don’t regenerate fast. Even after you stop the drug, it takes about a week for your body to make new, serotonin-filled platelets. So timing matters. Don’t just stop it the night before your procedure. Plan ahead.
What to Watch For
You don’t need to panic. But you do need to know the red flags:- Unexplained bruising, especially large patches without injury
- Nosebleeds that last longer than 10 minutes
- Bleeding gums when brushing teeth
- Passing black, tarry stools or maroon-colored stool
- Vomiting material that looks like coffee grounds
- Unusually heavy menstrual bleeding
If you see any of these, call your doctor. Don’t wait. These aren’t normal side effects-they’re warning signs.
New Tools Are Coming
Science is catching up. Researchers are now looking at genetics. A variation in the serotonin transporter gene (5-HTTLPR) can make some people way more sensitive to SSRI-induced bleeding. People with the S/S genotype have more than double the bleeding risk compared to those with L/L. In the next few years, doctors may start testing for this before prescribing SSRIs.There’s also early research on platelet-rich plasma infusions during surgery to counteract the effect. It’s experimental, but promising. And the European Medicines Agency is reviewing whether to update SSRI labels with genetic risk warnings by late 2025.
What Should You Do?
If you’re on an SSRI and worried about bleeding:- Don’t stop your medication on your own. Depression is dangerous too.
- Review your full medication list with your doctor-especially NSAIDs, aspirin, or blood thinners.
- If you’re at high risk, ask if switching to sertraline or citalopram is an option.
- Before any surgery or dental work, tell your provider you’re on an SSRI.
- Watch for signs of bleeding and report them immediately.
The goal isn’t to avoid SSRIs. It’s to use them safely. Millions of people take them without issue. But for those with risk factors, a smarter choice can make all the difference.
Can SSRIs cause internal bleeding?
Yes. SSRIs can increase the risk of internal bleeding, especially in the stomach and intestines. This is most common in people who also take NSAIDs, aspirin, or blood thinners. Signs include black or tarry stools, vomiting material that looks like coffee grounds, or sudden abdominal pain. If you notice these, seek medical help immediately.
Is sertraline safer than paroxetine for bleeding risk?
Yes. Sertraline has a much lower binding affinity for the serotonin transporter than paroxetine. Studies show paroxetine users have up to 50% higher risk of gastrointestinal bleeding compared to sertraline users. For patients with bleeding risk factors, sertraline is often the preferred SSRI.
Should I stop my SSRI before surgery?
It depends. For major surgeries like heart surgery, guidelines recommend continuing SSRIs to avoid depression relapse. For minor procedures with bleeding risk-like dental work or joint replacements-stopping the SSRI 5-7 days beforehand can reduce bleeding complications. Always talk to both your psychiatrist and surgeon before making any changes.
Can I take ibuprofen with an SSRI?
It’s not recommended. Combining NSAIDs like ibuprofen or naproxen with SSRIs increases bleeding risk by 4.5 times. Use acetaminophen (Tylenol) instead for pain relief. If you need an NSAID long-term, talk to your doctor about alternatives or protective medications like proton pump inhibitors.
Do all SSRIs affect platelets the same way?
No. SSRIs vary widely in how strongly they block serotonin reuptake. Paroxetine and fluvoxamine are the strongest and carry the highest bleeding risk. Sertraline and citalopram are weaker and safer for patients with bleeding concerns. The choice matters, especially if you have other risk factors.
Is there a test to check if my platelets are affected by SSRIs?
Standard blood tests won’t show it. Specialized platelet function tests can detect the dysfunction, but they’re not routine. The best approach is clinical: if you’re on a high-risk SSRI and have bleeding symptoms or other risk factors, your doctor should consider switching you to a safer option rather than testing.





Mark Rutkowski
12 November 2025 - 17:00 PM
It’s wild how a drug meant to heal the mind can quietly sabotage the body’s repair systems. Platelets aren’t just tiny blood cells-they’re the first responders to every cut, scrape, or internal tear. When SSRIs mute their serotonin signal, it’s like taking away their walkie-talkies in a fire drill. No one’s screaming, no one’s moving, and suddenly you’re bleeding out from a paper cut. We fixate on serotonin in the brain, but the body’s got its own language-and SSRIs are translating it wrong.
Ryan Everhart
13 November 2025 - 05:01 AM
so paroxetine is basically the aspirin of antidepressants then
David Barry
13 November 2025 - 07:59 AM
the data’s solid but the framing’s lazy. 18.7% bruising on paroxetine? That’s not a side effect-it’s a feature of the drug’s mechanism. You want mood stability? You get platelet instability. No free lunches. The real issue is that psychiatrists treat SSRIs like vitamins, not pharmacological scalpels. If you’re prescribing paroxetine to a 68-year-old on aspirin, you’re not treating depression-you’re playing Russian roulette with their GI tract.
Alex Ramos
13 November 2025 - 17:07 PM
Biggest takeaway: if you’re on an SSRI and you’re bruising like you’re in a bar fight, talk to your doc. Don’t wait for a nosebleed that won’t stop. I’ve seen patients ignore it until they ended up in the ER with a bleeding ulcer. Sertraline’s the quiet hero here-low risk, still effective. And if you’re on ibuprofen for your back pain? Swap it for Tylenol. It’s not glamorous, but it might save your life.
edgar popa
14 November 2025 - 13:50 PM
tylenol over ibuprofen duh
Eve Miller
14 November 2025 - 20:14 PM
It’s not just about switching SSRIs-it’s about recognizing that antidepressants are systemic drugs, not just brain chemicals. The FDA’s labeling is dangerously outdated. If you’re prescribing fluoxetine to someone with a history of ulcers and no mention of platelet risk, you’re negligent. This isn’t opinion-it’s clinical fact, backed by multiple meta-analyses. Why are we still acting like SSRIs are harmless?
Esperanza Decor
16 November 2025 - 16:01 PM
I’ve been on sertraline for three years and never had an issue-until last month. I woke up with a purple bruise the size of my palm on my thigh. No fall, no bump. I thought I was coming down with something. Then I remembered reading this exact study. I went to my doctor, asked about switching, and he said, ‘It’s probably nothing.’ But I pushed. Got a platelet function test. Turns out, my serotonin uptake was down 70%. He switched me to citalopram. Two weeks later, the bruising stopped. If you’re on any SSRI and noticing anything odd-don’t dismiss it. Your body’s trying to tell you something.
Deepa Lakshminarasimhan
17 November 2025 - 21:17 PM
they’re testing genes now? what’s next-mandatory DNA scans before you can get a prescription? they’re gonna start charging extra for serotonin variants. next thing you know, insurance will deny your SSRI because your 5-HTTLPR is ‘high risk.’ they’re turning mental health into a biotech lottery. they’ll sell you a ‘safe’ antidepressant and charge $800/month for the ‘low-bleeding’ version. wake up people, this is corporate medicine playing god.
Erica Cruz
19 November 2025 - 01:44 AM
Look, I get it. You’re all suddenly concerned about platelets. But let’s not pretend this is groundbreaking. This has been known since the 90s. The real scandal? That psychiatrists still prescribe paroxetine like it’s candy. It’s not ignorance-it’s inertia. Pharma reps push the ‘strongest’ SSRI because it sounds more effective. Doctors don’t want to admit they’ve been prescribing a bleeding risk to 80-year-olds for decades. The data’s been there. The warnings exist. But no one wants to change their script.
Alyssa Lopez
20 November 2025 - 01:54 AM
USA is the only country where you need a PHD to take an antidepressant. in russia we just take it and live. if you bleed you bleed. no one cares. why are we overcomplicating this? its just a pill. stop making it a crisis. also sertraline is for wusses. paroxetine is the real deal. if you can handle the bruising you can handle life.